Zika Virus Symptoms.
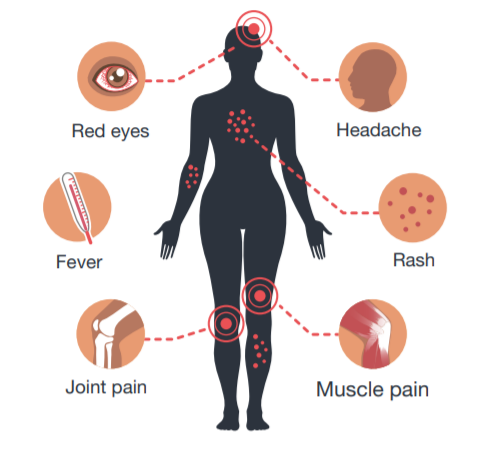
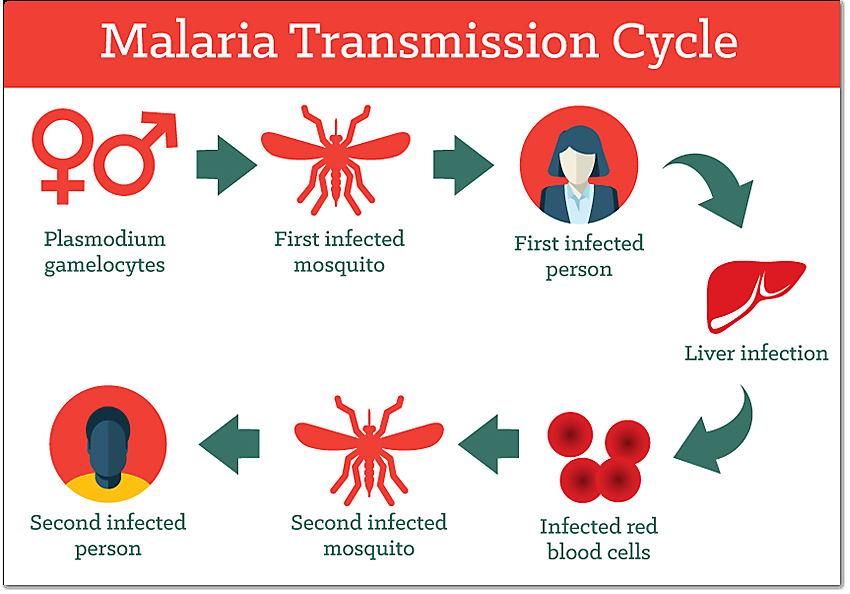
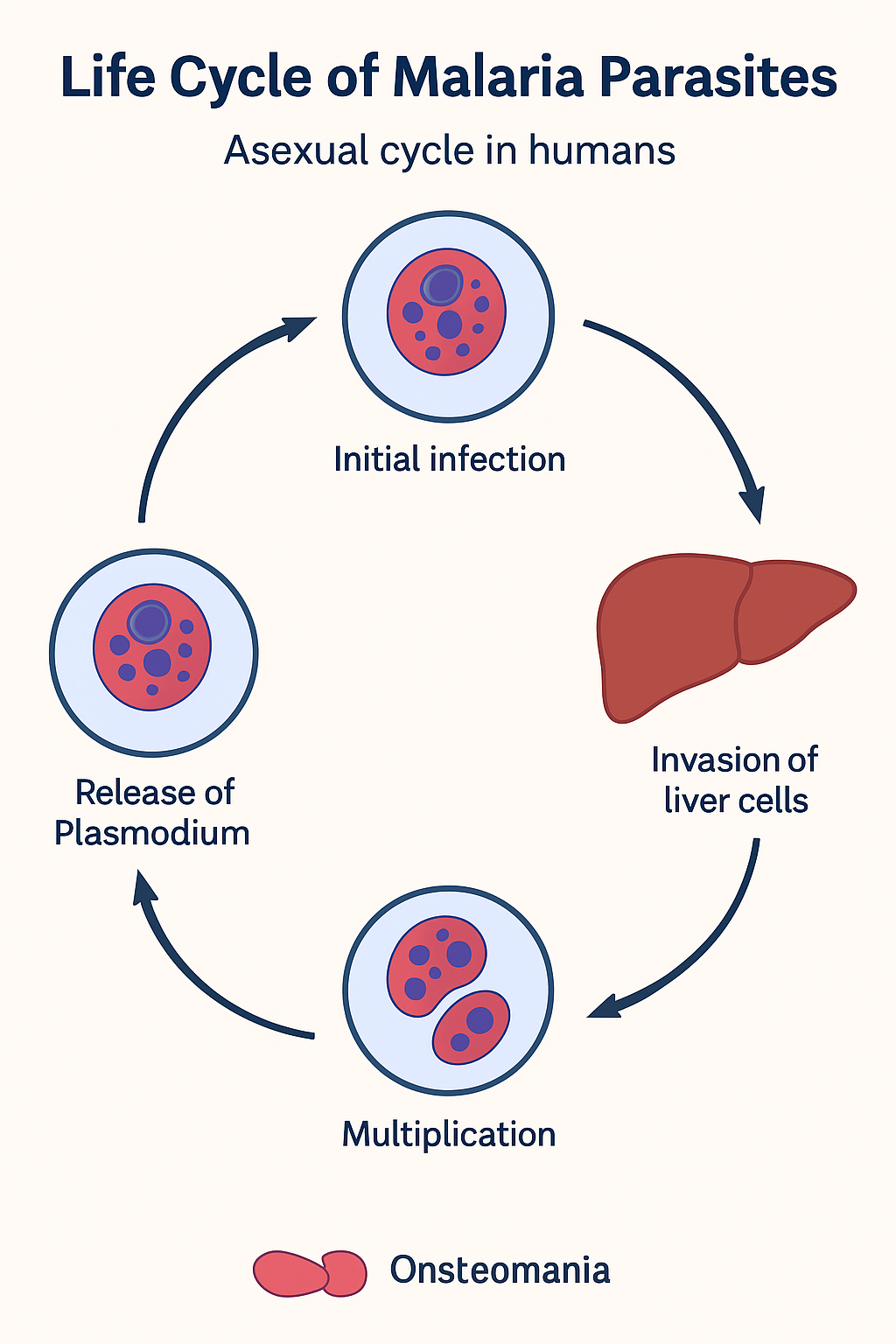
Zika virus is primarily transmitted by Aedes mosquitoes, which bite mostly during the daytime. Most people with Zika virus infection do not develop symptoms (up to 80% of people are asymptomatic). In symptomatic cases, the illness is usually mild and self-limiting. When symptoms occur, they include mild fever, rash, conjunctivitis, muscle and joint pain, malaise, and headache that last for 2 to 7 days. No vaccine is yet available for the prevention or treatment of Zika virus infection. Zika virus infection during pregnancy can cause.
Zika Virus Case Fatality and Severity in Present
Zika Virus Case Fatality and Severity in Present: –
Zika virus infections are typically mild or asymptomatic in adults and children, with no specific antiviral treatment available. Case fatality rates remain extremely low at around 0.1% or less for acute infections in non-pregnant individuals, based on reviews of confirmed cases. Severity is higher in vulnerable groups, such as fetuses from infected pregnancies leading to congenital Zika syndrome (CZS), where long-term child mortality can reach 14 to 52 deaths per 1000 person-years.
Current Global Trends
Current Global Trends: –
Transmission persists at low levels in the Americas, Asia, and Africa as of 2025, with over 25,800 suspected cases and one reported fatality in the Americas in 2025. In India, 151 cases were reported in 2024 across Maharashtra, Gujarat, and Karnataka, with no associated microcephaly or Guillain-Barre syndrome (GBS) death noted. Most infections, 60% to 80%, show no or mild symptoms like rash, fever, and joint pain lasting 2 to 7 days.
Severity in Adults
Severity in Adults:
Acute Zika rarely causes death or severe outcomes, with hospitalization in about 11% of symptomatic cases often linked to comorbidities or rare complications like GBS (0.3% of cases). GBS mortality in confirmed Zika-GBS cases is around 3%, with most recovering fully. Neurological issues like neuropathy or myelitis occur sporadically but are not typically fatal.
Risk in Pregnancy and Children
Risk in Pregnancy and Children:
Infection during pregnancy carries a 5 to 15% risk of congenital Zika syndrome (CZS) in infants, including microcephaly (reduced head size), leading to elevated early childhood mortality (e.g., 416 deaths per 10,000 person-years in Brazilian CZS cases vs. 29 in unaffected children). Causes include respiratory, infectious, and nervous system diseases with hazard ratios up to 57 times higher. No recent India-specific CZS fatalities reported.
Women aged 20 to 49 show higher reported Zika virus disease incidence due to a mix of behavioral, biological, and reporting factors. Women in this reproductive age group often seek healthcare more frequently for mild symptoms like rash or fever, leading to higher testing and confirmation rates compared to men. Greater domestic exposure to Aedes mosquitoes during daily activities at home contributes to increased bites. Sexual transmission, potentially male to female, elevates risk in sexually active individuals.
Biological and Reporting Biases
Biological and reporting biases:
Pregnancy-related concerns prompt more diagnostic testing among women of childbearing age, amplifying reported cases even among nonpregnant individuals. Symptomatic disease may manifest differently, with women more likely to develop noticeable symptoms prompting care. Among suspected cases in older adults (>40 years), women test positive more often than men.
Severity of Congenital Zika Syndrome (CZS)
Severity Of CZS:-
Congenital Zika syndrome (CZS) remains a severe, lifelong condition primarily affecting the central nervous system of infants born to Zika-infected mothers, with complications persisting into childhood and beyond. Recent 2025 studies from Brazil highlight elevated mortality risks, while core clinical features like microcephaly drive profound disabilities.
Core Clinical Features of CZS
Core Clinical Features: –
CZS manifests as microcephaly, brain calcifications, limb contractures, hypertonia, and eye abnormalities, e.g., chorioretinal atrophy and hearing loss in 5% to 15% of exposed fetuses. Infants often show irritability (85%), seizures (50%), dysphagia (15%), and hypotonia, leading to feeding difficulties and growth failure. Arthrogryposis and cerebellar hypoplasia contribute to mortality impairments from birth.
Mortality Risks Associated With CZS
Mortality Risks:-
Children under 5 with CZS face 13-fold higher all-cause mortality (HR 13.10), escalating to 17-fold when excluding preterm/low birth weight cases. Leading causes include respiratory diseases (HR 30), infectious/parasitic (HR 28), and nervous system disorders (HR 57), often from aspiration pneumonia due to dysphagia or epilepsy. By ages 2–3, risks amplify to 45 to 100 times higher for specific causes.
Long-Term Complications
Long-Term Complications:
Eight years post-outbreak, survivors exhibit severe functional limits: >60% have poor visual function, major mobility issues, and feeding dependencies. Neurodevelopmental delays affect motor (IRR 3.4) and cognitive domains (IRR 4.7), with epilepsy, blindness, and poor seizure control common. Multidisciplinary care is essential, yet gaps persist in global support protocols.