Thyroid cancer is a malignancy originating in the thyroid gland, a butterfly-shaped organ in the neck that produces hormones regulating metabolism. It develops when thyroid cells grow uncontrollably and can spread to other body parts.
Definition
Thyroid cancer involves abnormal cell growth in the thyroid gland’s tissues. It is classified based on the affected cells and their differentiation level.
Causes and Risk Factors
Key risk factors include exposure to ionizing radiation, especially in childhood, such as from nuclear accidents or medical treatments. Other factors encompass family history of thyroid diseases, genetic syndromes like multiple endocrine neoplasia, obesity, and benign thyroid conditions like goiter or thyroiditis.
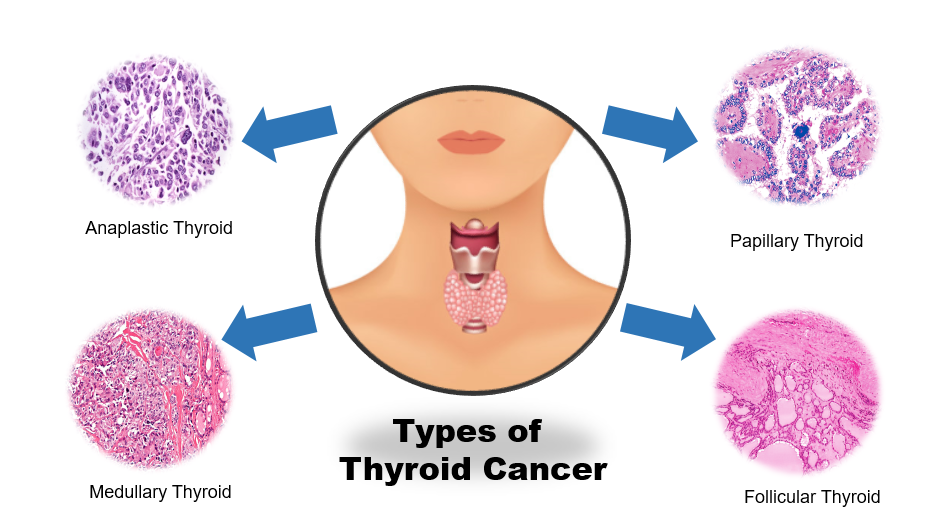
Main Types of Thyroid Cancer
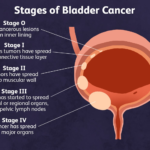
Thyroid cancer is generally classified into four main types. These arise from different cells in the thyroid gland and vary in aggressiveness and prevalence.
1) Papillary: Most common (80% to 85% of cases), slow-growing, excellent prognosis.
2) Follicular: Second most common (10% to 15%); can spread to distant sites like lungs or bones.
3) Medullary: 4% to 10% of cases originate from C-cells, often linked to genetic syndromes.
4) Anaplastic: Rare (< 2%), very aggressive, and fast-spreading.
5) Additional Categories: Rare subtypes include Hurthle cell (oncocytic, a follicular variant) and poorly differentiated carcinomas per 2022 WHO updates. Over 10 to 15 histological subtypes exist within these, but four represent the primary clinical categories.
Prevalence Table
| Type | Prevalence |
|---|---|
| Papillary | 80% to 85% |
| Follicular | 10% to 15% |
| Medullary | 4% to 10% |
| Anaplastic | < 2% |
Symptoms
Early stages often show no symptoms, but a painless neck lump, hoarseness, difficulty swallowing, neck pain, or cough may appear as it progresses.
Diagnosis
Diagnosis starts with clinical evaluation of neck lumps. Confirmation relies on biopsy results and imaging to assess spread.
Diagnostic Methods
Ultrasound is the first-line imaging for nodules and lymph nodes, guiding fine-needle aspiration (FNA) biopsy. Additional tools include CT/MRI scans, blood tests for tumor markers (e.g., calcitonin for medullary type), and radioactive iodine scans.
Prevention Measures
No guaranteed prevention exists, but minimizing radiation exposure, maintaining a healthy weight, having a balanced diet with adequate iodine, doing physical activity, and avoiding obesity help reduce risk. Potassium iodide protects against radioactive iodine in nuclear events.
Control Measures
Early detection via screening high-risk groups (e.g., radiation exposed), regular monitoring, and prompt treatment control spread. Public health screening policies balance benefits against harms like overdiagnosis. Active surveillance is recommended for very small, low-risk papillary thyroid microcarcinomas (PTMCs) typically less than 1 cm in size. This approach avoids immediate surgery for indolent tumors confined to the thyroid without lymph node involvement, extrathyroidal extension, or metastasis, allowing close monitoring instead. Regular ultrasound every 6 months initially, then annually, plus physical examination and TSH suppression if needed. Switch to surgery if there is growth, lymph node appearance, or patient preference.
Treatment
Surgery (thyroidectomy) is primary, often followed by radioactive iodine therapy, thyroid hormone suppression, targeted therapy, or external radiation. Chemotherapy is less common; watchful waiting suits low-risk cases.
Standard Treatments for Papillary Thyroid Cancer
Standard treatments for papillary thyroid cancer center on surgery as the cornerstone, often followed by adjuvant therapies. This highly treatable cancer typically responds well to a combination of thyroid removal, radioactive iodine, and hormone replacement. Total thyroidectomy removes the entire thyroid gland and is the most common approach for most cases. Lobectomy (removing only the affected lobe) may suffice for very small, low-risk tumors. Central neck dissection addresses lymph node involvement.
Public Awareness and Community Engagement
Public Awareness: Campaigns emphasize neck lump checks and early detection, using media, celebrities, and events to educate on symptoms and risks. Studies show gaps in knowledge of risk factors and screening.
Community Engagement: Online health communities and events foster patient support, information sharing, and research participation. Partnerships between charities, hospitals, and locals boost turnout and awareness.
IEC Materials: Information, Education, and Communication tools include posters, booklets, social media graphics, and radio/print ads promoting “get your neck checked.” These highlight lumps, prevention, and early treatment benefits.
Role of Public Health Department: The department runs awareness campaigns, screens for at-risk populations, has a policy on radiation protection, and integrates thyroid health into primary care. They promote education, monitor incidence, and support research to address gaps.
Prognosis and Survival Rates for Papillary Thyroid Cancer
Papillary thyroid cancer has an excellent prognosis overall. It is the most common and treatable form of thyroid cancer, with survival rates exceeding 99% for localized cases.
Prognosis Factors
Prognosis improves for younger patients under 40, smaller tumors, and cases confined to the thyroid. Poorer outcomes are linked to age over 55, distant metastasis, large tumors (>4 cm), or extrathyroid spread.
Survival Rates
Localized (confined to thyroid): 99%, 5-year survival
Regional (nearby lymph nodes/structures): 98-99%, 5-year survival
Distant metastasis: 50-75%, 5-year survival
Overall: >99% 5-year, >90% 10-20-year survival.
Thyroid Cancer Types and Risk Factor Links
Thyroid cancer risk factors vary by type, with radiation exposure common across differentiated types like papillary and follicular.
| Type | Main Risk Factors |
|---|---|
| Papillary | Radiation (childhood), obesity, genetics (FAP/Cowden), Female |
| Follicular | Iodine deficiency, radiation, Cowden/Werner |
| Medullary | RET mutations (MEN2), hereditary syndromes. |
| Anaplastic | Prior thyroid cancer, age, and genetic mutations. |
The Effect of Iodine Supplementation
Iodine deficiency plays a stronger role in follicular thyroid cancer than other types, increasing its incidence while favoring papillary dominance in iodine-sufficient areas. It triggers chronic TSH elevation, promoting follicular cell hyperplasia and malignant transformation, particularly in endemic regions.
Follicular Thyroid Cancer and Iodine Deficiency
Follicular Thyroid Cancer: Strongly associated with iodine deficiency; low intake leads to higher follicular carcinoma rates (up to 5 to 10 times vs. papillary ratio in deficient areas.) Iodization programs reduce incidence, with studies showing the P:F ratio shifting from 1:1 to 3-6:1 post-supplementation.
Iodine Deficiency Table
| Type | Iodine deficiency |
|---|---|
| Follicular | High (increases incidence via TSH) |
| Papillary | Low (minimal influence) |
| Medullary/ Anaplastic | None |
Mechanism Of Iodine
Iodine is essential for thyroxine (T4) and triiodothyronine (T3) production; deficiency limits hormone synthesis, reducing circulating T4/T3 levels. The pituitary responds by thyroid, causing persistent hyperplasia. Chronic TSH elevation acts as a growth on follicular cells via TSH receptors, inducing proliferation, goiter, and nodular changes—precursors to FTC.
Low/lack of Iodine → Reduced T3/T4 (synthesis)
Pituitary Response → TSH secretion
Thyroid Impact → Hyperplasia → FTC risk
Thyroid Dysfunction and Cancer Risk
Neither hyperthyroidism nor hypothyroidism directly causes thyroid cancer. While elevated TSH from hypothyroidism (often due to iodine deficiency or Hashimoto’s) is a growth promoter for follicular cells and links to higher thyroid cancer risk via chronic stimulation, these thyroid dysfunctions are risk factors rather than direct causes.