Stomach (Gastric) Cancer
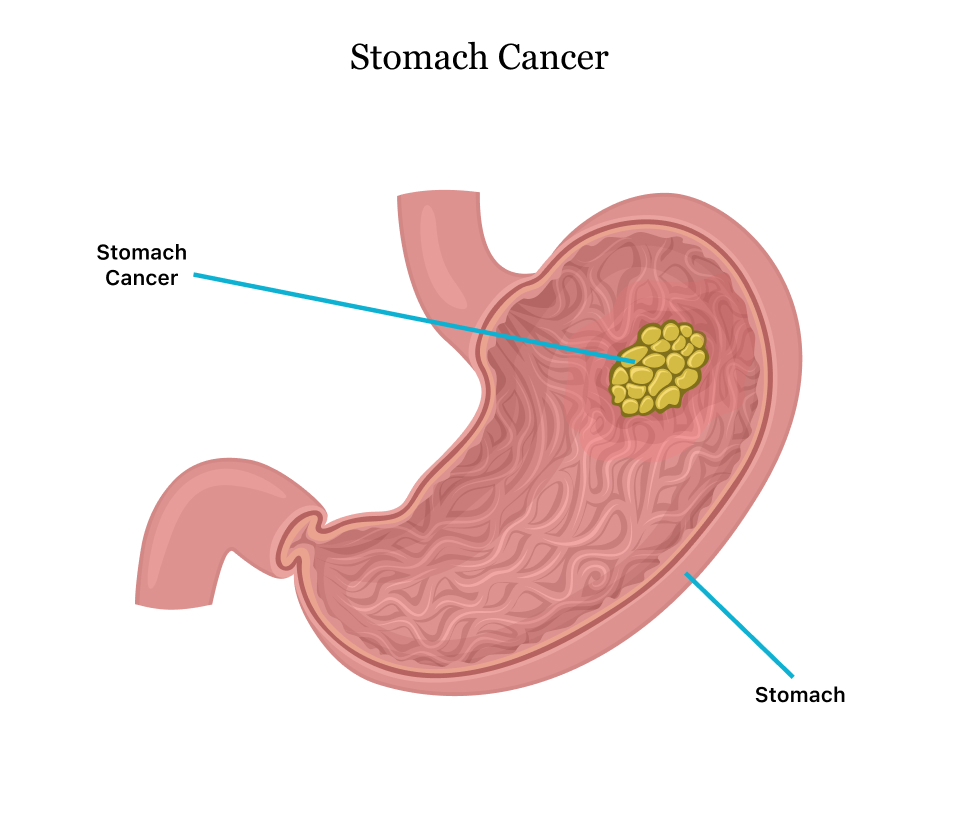
Stomach cancer, also known as gastric cancer, is a disease where cells in the stomach lining grow uncontrollably, forming tumors that can invade nearby tissues or spread elsewhere.
Definition
Stomach cancer begins in the inner lining of the stomach and develops slowly over years due to DNA changes causing cells to multiply rapidly and form tumors. It most often starts in mucus-producing cells (adenocarcinoma, ~95% of cases) but can arise from other cell types.
Causes
DNA mutations in stomach cells, triggered by factors like H. pylori infection, lead to uncontrolled growth. Chronic inflammation (gastritis), polyps, or prior stomach surgery contribute; exact triggers remain unclear.
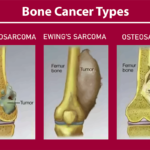
Main Types of Stomach Cancer
Adenocarcinoma: Most common, from glandular mucus cells
Gastrointestinal stromal tumors (GIST):- From nerve cells in the stomach wall.
Lymphomas, carcinoid tumors, and sarcomas are rare and come from immune, neuroendocrine, or connective tissues.
Symptoms
Early symptoms are often absent; later ones include indigestion, stomach pain, bloating after small meals, nausea, vomiting, unintentional weight loss, fatigue, and black stools. Advanced cases may cause swallowing difficulty or blood in vomit/stools.
Diagnosis
Diagnosis starts with upper endoscopy (camera down throat to view stomach) and biopsy for cell analysis. Staging uses CT/PET scans, endoscopic ultrasound, blood tests, or laparoscopy to check spread.
Diagnosis Methods: –
Endoscopy with biopsy: Primary method
Imaging: CT, PET, ultrasound for staging
Blood tests: for tumor markers or liver function.
Prevention Measures
Eat more fruits/vegetables, limit salty and smoked foods, quit smoking, and treat H. pylori infections. High-risk individuals (family history, genetic syndromes) may need screening endoscopy.
Control Measures
Primary: Reduce risks via lifestyle/diet changes.
Secondary: Early screening in high-prevalence areas.
Tertiary: Manage advanced cases to prolong life.
Treatment
Surgery (partial / total gastrectomy, lymph node removal) for early stages.
Chemotherapy (systemic or HIPEC).
Radiation, targeted therapy.
Immunotherapy for advanced.
Palliative care relieves symptoms.
Public Awareness
Campaigns educate on risks (H. pylori, diet), symptoms (bloating, weight loss), and screening via online modules, media, and community programs to boost early detection. Awareness improves in targeted regions, but gaps persist in low-socioeconomic groups.
Community Engagement
Involves sensitization on symptoms/risks, support groups, and lifestyle workshops; survivors share stories online/in person to encourage screening. Programs target high-risk areas like East Asia.
IEC Materials
Information, education, and communication tools include posters, videos, brochures on symptoms, prevention (e.g., NHM India materials), online modules, and infographics for schools/communities.
Role of Public Health Department
Develops screening programs, funds H. pylori eradication, runs awareness campaigns (e.g., Be Clear on Cancer), monitors incidence, and integrates into NCD frameworks like India’s NP-NCD for policy, training, and resource allocation.
Stomach Cancer Survival Rates and Prognosis
Stomach cancer survival rates vary widely by stage at diagnosis, with overall 5-year relative survival around 35% to 40% based on recent U.S. data from people diagnosed from 2015 to 2021. Prognosis improves dramatically with early detection but worsens if the cancer has spread.
Survival Rates
The 5-year relative survival rate for all stages combined is approximately 37.9%, meaning people with stomach cancer are about 38% as likely as those without it to live 5 years post-diagnosis. Rates have improved over time due to better treatments, reaching up to 71% in some centers for 2018-2022 cases.
Survival by Stage
By Stage:-
| Stage | 5-Year Relative Survival Rate | Description |
|---|---|---|
| Localized | 75% to 80% | Cancer confined to stomach |
| Regional | 53% to 40% | Spread to nearby lymph nodes |
| Distant | 5% to 10% | Metastasized to distant sites |
Factors Affecting Prognosis
Age, overall health, tumor biology, lymph node involvement, and treatment response influence outcomes; surgery boosts early-stage survival to 75% to 85%. Newer therapies like immunotherapy improve advanced cases, but late diagnosis remains common.
Stages of Stomach Cancer
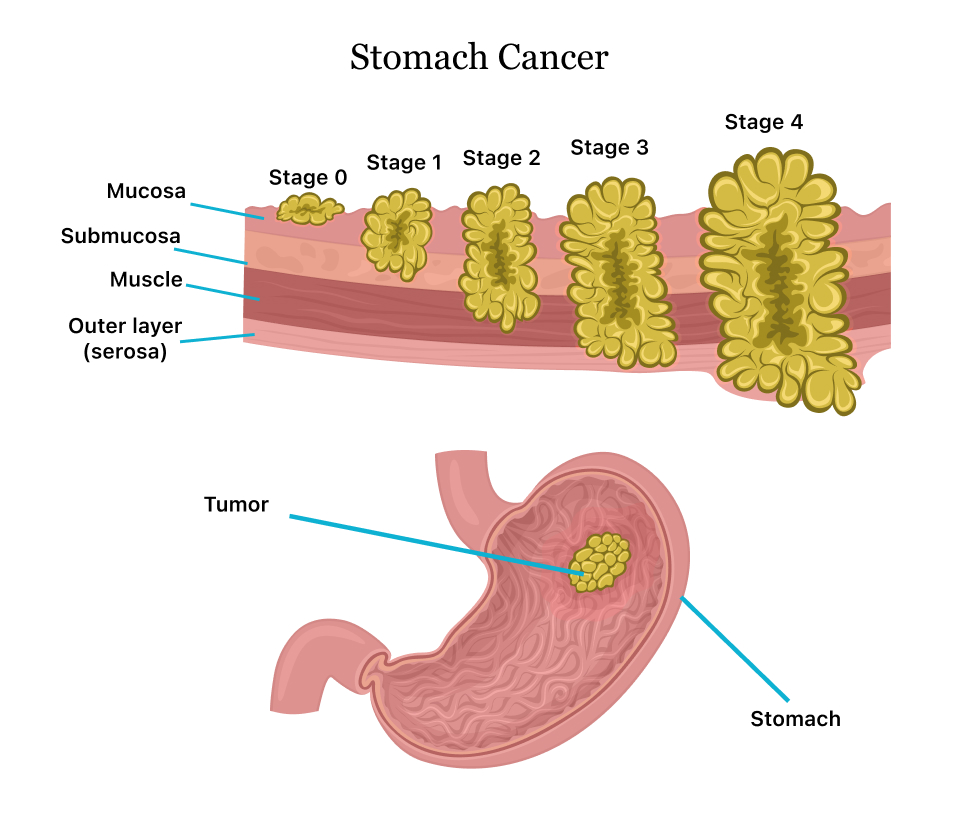
Stomach cancer, also known as gastric cancer, is staged using the TNM system to assess tumor size (T), lymph node involvement (N), and metastasis (M). Staging ranges from 0 to IV and guides treatment options.
Stage 0
Stage 0:-
Cancer is confined to the innermost lining (mucosa) without invading deeper layers or spreading. It’s also called carcinoma in situ.
Stage 1
Stage 1: Divided into IA and IB.
IA: Cancer invades the mucosa or submucosa but not lymph nodes.
IB: Cancer reaches the muscle layer or involves 1-2 nearby lymph nodes.
Stage 2
Stage 2: Divided into IIA and IIB.
IIA: Cancer in submucosa with 3-6 lymph nodes, muscle layer with 1-2 nodes, or subserosa.
IIB: Deeper invasion with more nodes (e.g., submucosa with 7-15 nodes or serosa penetration).
Stage 3
Stage 3: Advanced local spread, divided into IIIA, IIIB, and IIIC.
IIIA: Muscle layer with 7-15 nodes, subserosa with 3-6 nodes, or nearby organ invasion.
IIIB: Various combinations like serosa with 7-15 nodes or organ invasion with 1-6 nodes.
IIIC: Serosa with 16+ nodes or organ invasion with 7+ nodes.
Stage 4
Stage 4:-
Cancer has metastasized to distant sites like the liver, lungs, or fat lymph nodes. Treatment focuses on palliation.
Difference Between the Stomach Cancer and Colorectal Cancer
Difference between the the stomach cancer and colorectal cancer:-
Stomach cancer and colorectal cancer differ in their location, symptoms, risk factors, and prognosis, though both are gastrointestinal malignancies.
Location: Stomach cancer originates in the stomach lining, often mucus-producing cells in the upper abdomen, while colorectal cancer starts in the colon or rectum, the large intestine’s lower parts.
Symptoms:—Stomach cancer typically causes upper abdominal pain, early satiety, nausea, vomiting after small meals, black stools, and swallowing issues, while colorectal cancer features rectal bleeding, blood in stools, bowel habit changes, and cramping, without prominent nausea or swallowing problems.
Risk factors: Stomach cancer is strongly linked to H. pylori infection, salty/smoked foods, smoking, and family history, while colorectal cancer is associated with polyps, low-fiber diet, obesity, inactivity, and genetic syndromes like Lynch.
Prognosis: Stomach cancer has lower survival rates than colorectal cancer across stages, influenced mainly by metastasis; tumor grade affects colorectal more. Early colorectal detection via colonoscopy yields better outcomes (up to 90% 5-year survival localized) versus stomach cancer’s ~70%.