Skin cancer refers to uncontrolled growth of abnormal skin cells, most often due to DNA damage from ultraviolet (UV) radiation exposure. It is the most common cancer worldwide, with non-melanoma types (basal cell carcinoma and squamous cell carcinoma) far outnumbering melanoma, which is deadlier but less common.
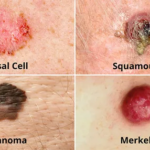
Types:
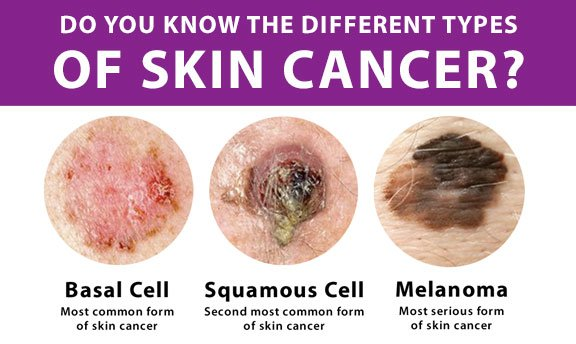
Basal cell carcinoma (BCC, ~80%):
Slow-growing, forms basal cells in epidermis, rarely metastasizes, and appears as a pearly nodule or sore.
Squamous cell carcinoma (SCC, ~20% ):
From squamous cells; more aggressive, can spread; presents as a scaly red patch or wart.
Melanoma (~1% but deadliest):-
From melanocytes; highly metastatic; irregular mole (ABCDE: asymmetry, border irregularity, color variation, diameter > 6 mm, evolving).
Rare types:
Merkel cell, cutaneous T-cell lymphoma.

Causes and Risk Factors: –
Primary causes are UV exposure from the sun or tanning beds or lamps; fair skin, many moles, family history, weakened immunity, and prior sunburns increase risk. Unlike cervical cancer’s viral cause, skin cancer links to cumulative UV damage, not HPV primarily (though beta-HPV types may contribute in immunosuppressed people).
Symptoms:-
New growths, sores that don’t heal, changing moles, itchy/bleeding spots, or rough/scaly patches. Early detection via self-exam and dermatologist checks is key.
Lab Diagnosis:-
Skin biopsy (shave, punch, excisional) confirms type/stage: staging uses TNM (tumor size, nodes, metastasis) for melanoma (0-IV). Dermoscopy or imaging aids.
Screening Methods:-
No routine population screening (USPSTF “I” grade due to insufficient mortality evidence); high-risk self-exams monthly (ABCDE rule) and annual dermatologist checks recommended. Visual full-body exams; emerging AI dermoscopy.
Prevention Measures:-
Use broad-spectrum SPF 30+ sunscreen daily, seek shade from 10 am to 4 pm, wear protective clothing/hat/sunglasses, and avoid tanning beds. Public campaigns like “Slip, Slap, Slop” promote awareness; there is no vaccine routine like HPV.
Control Measures: –
Sun-safety campaigns, early detection education, occupational UV protection (e.g., outdoor workers), and tobacco avoidance (lip SCC). Treat precancers (actinic keratosis) with topical fluorouracil.
Treatment by Type/Stage:-
Early BCC/SCC:-
Surgery (excision, Mohs for precision), cryotherapy, topical creams (5-FU, imiquimod).
Advanced:-
Radiation, targeted therapy (cemiplimab for PD-L1+), and immunotherapy.
Melanoma:-
Wide excision: sentinel node biopsy; stage III/IV: immunotherapy (pembrolizumab), targeted (BRAF inhibitors). Cure rates are near 100% for early detection.
Public Awareness: –
Campaigns highlight UV risks, the ABCDE self-exam, and sunscreen myths via media/social media; India focuses on rising incidence in high-altitude areas (e.g., Shimla, Kangra) amid urbanization/climate change.
Community Engagement:
Local drives with ASHA workers, rural camps, and school-based programs for self-exams and sun safety; initiatives like “Radiant Health“ in Himachal Pradesh build knowledge on risks and prevention.
IEC Materials:
Posters, pamphlets, and videos in regional languages on symptoms, sunscreen use, and self-exam steps; visuals of ABCDE, tailored for low-literacy via NPCDCS and NHM modules.
Role of Public Health Department: –
India’s MoHFW, NHM integrates via NPCDCS: awareness IEC, training PHC, CHC, staff, dermatologists, high-risk screening pilots, tobacco control (NTCP for SCC), and surveillance; it collaborates with NGOs for camps in UV-prone areas like the Maharashtra highlands.
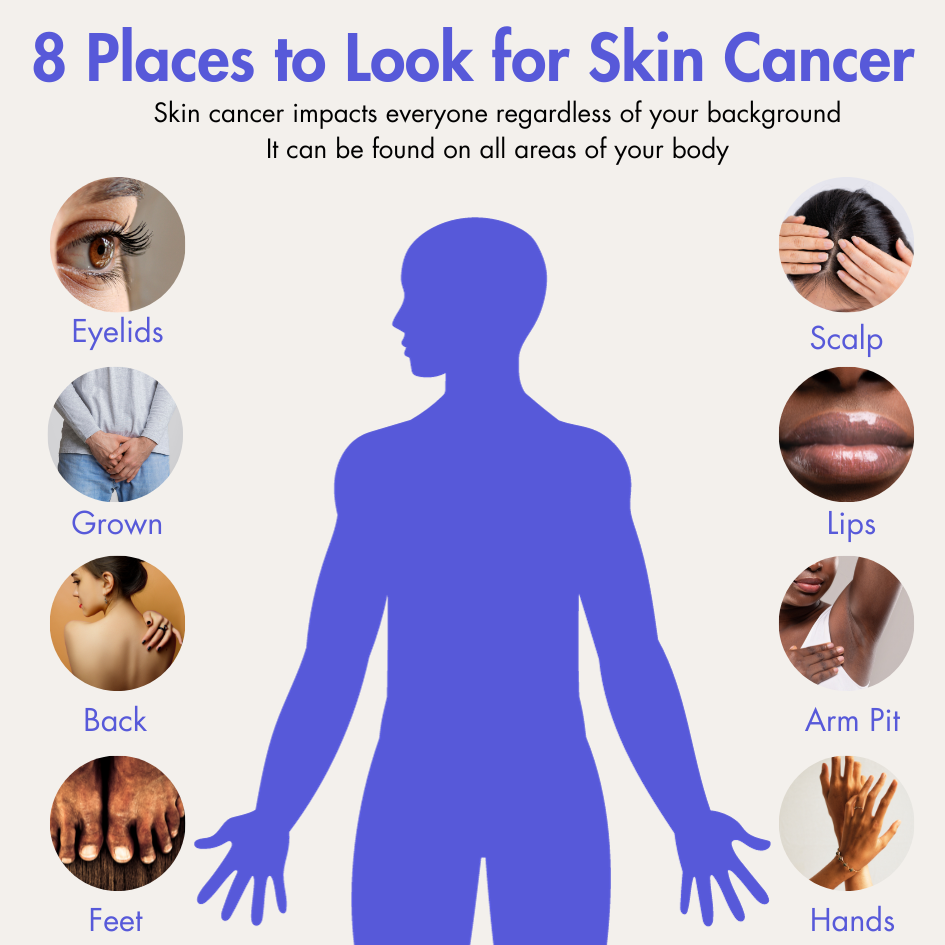
Procedure For Performing Skin Self-Exams:-
Skin self-exams help detect skin cancer early by systematically checking your body monthly. Use good lighting, a full-length mirror, a hand mirror, a comb or blow dryer, and a partner if possible for hard-to-see areas. Track changes with photos or notes.
Preparation:-
Examine your skin once a month after a shower when pores are open and skin is relaxed. Remove all clothing and polish-free nails. Learn your skin’s normal pattern of moles, freckles, and marks on the first exam to spot changes later.
Step-by-Step Procedure: –
Follows this head-to-head order for thorough coverage.
Face and Scalp:-
Check face, nose, lips, mouth, ears (front and back), and scalp; use a comb or blow dryer to part hair.
Hands and arms:
Inspect palms, backs, between fingers, under nails, elbows, underarms, and sides.
Torso front:
Examine neck, chest, abdomen, and sides; women lift breasts to check underneath.
Back and buttocks:
Use a hand mirror for shoulders, neck, back, buttocks, and genitals.
Legs and feet:
Check thighs, shins, calves, tops/bottoms of feet, between toes, and under toenails.
ABCDE Rule For Suspicious Spots:-
Look for changes in this guide for moles or lesions.
| Feature | Description |
| A: Asymmetry | One half unlike the other |
| B: Border | Irregular, ragged, or blurred edges |
| C: Color | Varied shades (brown, black, red, white, blue) |
| D: Diameter | Larger than 6 mm (pencil eraser size) |
| E: Evolving | Changes in size, shape, color, or symptoms like itching and bleeding. |
When to See a Doctor: –
Consult a dermatologist for any ABCDE matches, new growths, sores that don’t heal, or personal or family history of skin cancer. Track changes with photos or a mole map.