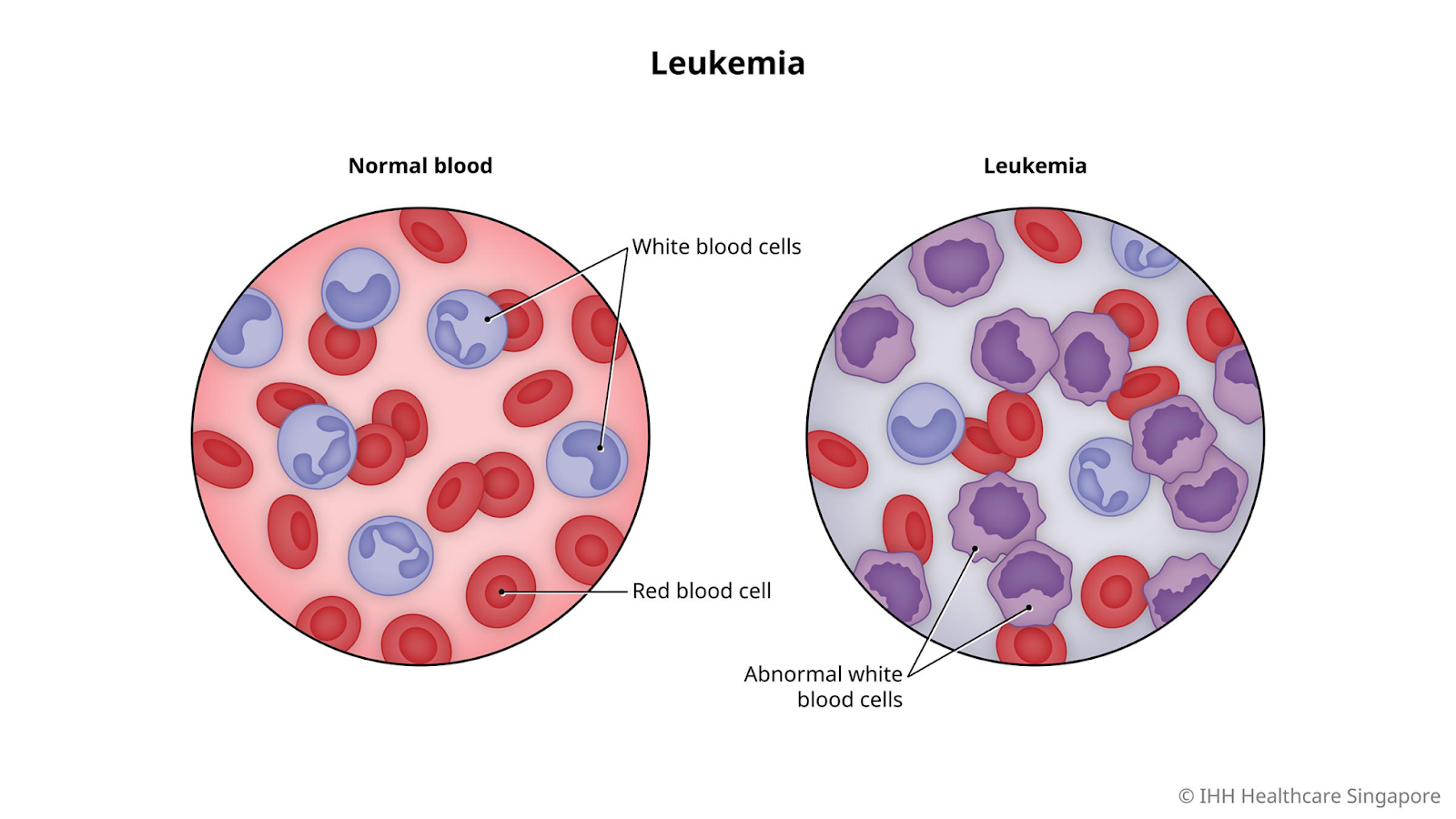
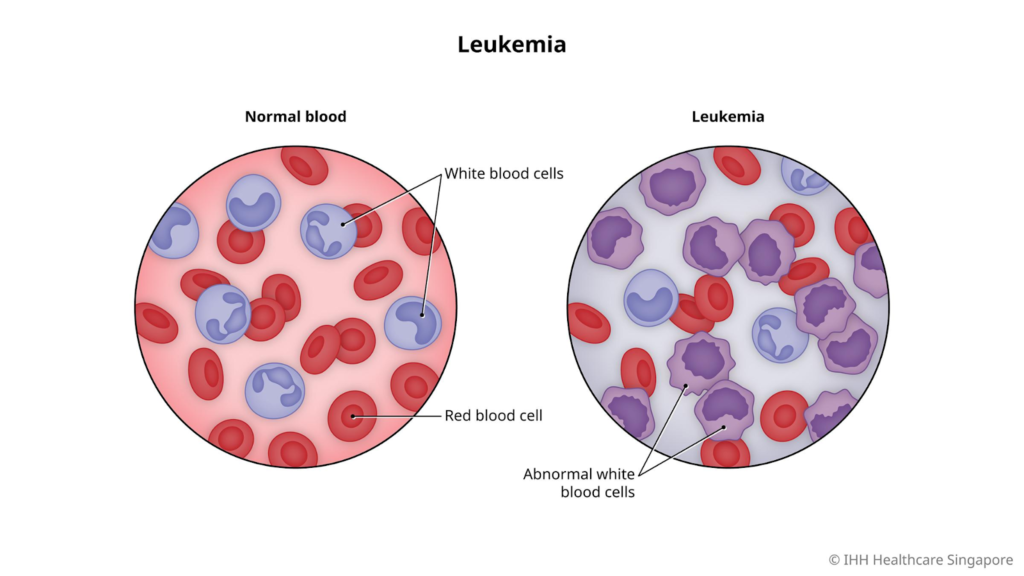
Leukemia, or blood cancer, is a malignancy affecting blood-forming tissues in the bone marrow and blood. It leads to overproduction of abnormal white blood cells that impair normal blood cell function and immunity.
Definition
Definition: Leukemia is cancer of the blood and bone marrow where immature white blood cells multiply uncontrollably, crowding out healthy cells. This disrupts red blood cell, platelet, and mature white blood cell production, increasing infection, bleeding, and anemia risks.
Causes
Causes: Exact causes are unknown, but risk factors include genetic mutations in bone marrow DNA, radiation or chemical exposure (e.g., benzene), prior chemotherapy, smoking, and genetic conditions like Down syndrome. Family history and certain viruses may contribute in some cases.
Main Types of Leukemia
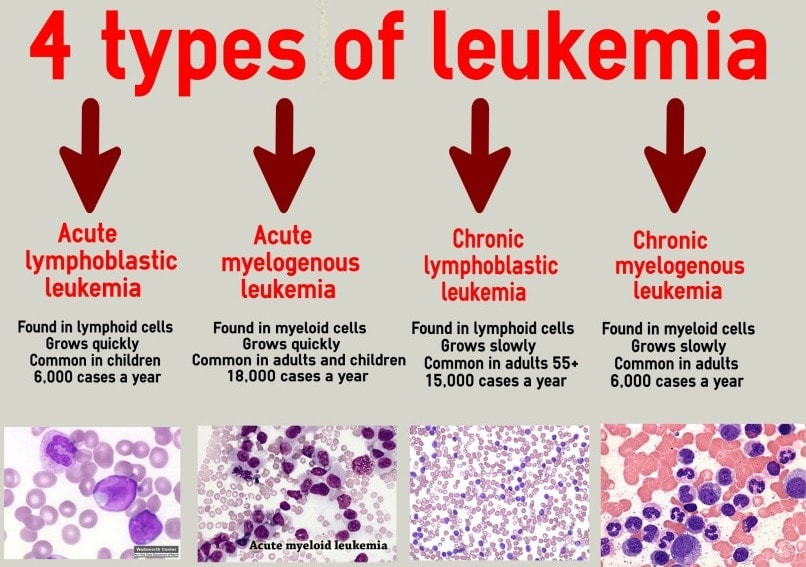
Main Types:
Acute Lymphoblastic Leukemia (ALL)
Fast-growing, common in children, and affects lymphoid cells.
Acute Myeloid Leukemia (AML)
Rapid, affects myeloid cells, more common in adults.
Chronic Lymphocytic Leukemia (CLL)
Slow-growing, mainly in older adults, lymphoid origin.
Chronic Myeloid Leukemia (CML)
Slow initially, myeloid cells, often in adults.
Symptoms
Symptoms: Common signs include fatigue, fever, frequent infections, easy bruising/bleeding, bone pain, swollen lymph nodes, enlarged spleen/liver, weight loss, and shortness of breath. Chronic types may be asymptomatic early on.
Diagnosis and Methods
Diagnosis and Methods: Diagnosis starts with a complete blood count (CBC) showing abnormal cell counts, followed by blood smear microscopy and flow cytometry to identify cell types. Bone marrow biopsy/aspiration confirms subtype; imaging (CT, MRI, PET) checks spread. Genetic tests detect mutations like FLT3.
Prevention Measures
Prevention Measures: No sure prevention exists, but avoid tobacco, limit radiation and chemical exposure (e.g., benzene), vaccinate against hepatitis B/HPV, and maintain a healthy weight. Early screening for high-risk groups aids secondary prevention.
Control Measures
Control Measures: Public health focuses on early detection via screening in NCD programs, risk factor reduction, and treatment access to prevent progression. In India, NPCDCS integrates leukemia into NCD clinics for diagnosis, drugs, and referral.
Treatment
Treatment:—Options include chemotherapy (induction, consolidation, maintenance phases), targeted therapy (e.g., tyrosine kinase inhibitors for CML), immunotherapy (e.g., CAR-T), radiation, and stem cell transplant. Treatment varies by type, age, and genetics; supportive care manages side effects.
Public Awareness
Public Awareness: Campaigns emphasize early symptoms, risk factors, and screening to reduce stigma and delays, using vernacular materials and community outreach. In India, integrate into NCD education via ASHAs and media.
Community Engagement
Community Engagement: Involve ASHAs workers, Anganwadi staff, and influencers for grassroots education, especially in rural/low-literacy areas; school-based programs and events build knowledge on monitoring/recurrence.
IEC Materials
IEC Materials: – Uses leaflets, banners, videos, and posters in local languages. e.g., Marathi, Hindi, Urdu, Kannada, Telugu, etc., visual aids on symptoms, screening; integrate into NPCDCS for cancer kits.
Role of Public Health Department
Role of Public Health Department: In India, under NPCDCS, MoHFW, departments establish NCD cells and clinics at district, CHC, PHC, and SC levels for free diagnostics, drugs, cardiac/cancer day care, and referrals. They promote screening age 30+, train workers, fund infrastructure, and drive awareness via Ayushman Bharat. Focus on high-burden cancers like leukemia via surveillance and resource allocation.
Leukemia Survival Rates
Leukemia Survival Rates: Leukemia survival rates vary widely by type, age, genetics, and treatment response, with an overall 5-year relative survival rate around 65% to 70% across all types. Acute forms generally have lower rates than chronic ones, and staging is less standardized than in solid tumors—often based on blood counts, cell maturity, organ involvement, or risk groups rather than traditional stages. I-IV.
Survival by Types
Survival by Types:-
Acute Lymphoblastic Leukemia (ALL)
Overall 5-year rate is 70% to 75% higher in children (90%+ for under 20) due to better chemotherapy response and drops to 30% to 40% in adults over 60.
Acute Myeloid Leukemia (AML)
The overall 5-year rate is 30% to 35%; favorable genetics boost it to 50% to 70%, while poor risk cases fall below 20%, worse in the elderly (under 10% for 65+).
Chronic Lymphocytic Leukemia (CLL)
Highest at 85% to 90% overall 5-year rate; early-stage (Rai 0-I) exceeds 90%; advanced (III-IV) is around 20% to 50%; indolent progression aids survival.
Chronic Myeloid Leukemia (CML)
70% overall 5-year rate; TKIs like imatinib push the chronic phase to 90%+, but the blast crisis drops to 10% to 20%.
Survival Rates for Leukemia in Children Against Adults
Survival rates for leukemia in children against adults:
Children with leukemia have significantly higher survival rates than adults, primarily due to better treatment responses, optimized pediatric protocols, and biological differences in disease behavior.
Overall 5-year survival for childhood leukemia exceeds 90%, with Acute Lymphoblastic Leukemia (ALL) at 90% to 95%.
Adults (Ages 20+):- Adult overall 5-year survival is around 40% to 65% across types, far lower than children. ALL drops to 30% to 45% for ages 20% to 30% and further with age, while AML is 20% to 30% overall and under 10% for those 65+. Chronic types like CLL fare better at 90% but still lag pediatric acute cures.
Key Comparisons:
| Type | Children (0 to 19 yrs, yr) | Adults (20+ yrs, 5 yrs) |
| ALL | 90% to 95% | 30% to 70% (age dependent) |
| AML | 70% to 71% | 20% to 35% |
| Overall | > 90% | 65% |
Survival gaps widen with age due to comorbidities, resistance, and less intensive therapies; adolescents (15-25) bridge the divide at 75% to 90%.