Colorectal cancer, also known as colon or bowel cancer, is a malignancy that develops in the colon or rectum, parts of the large intestine, often from uncontrolled growth of epithelial cells.
Definition
Colorectal cancer arises from the inner lining of the colon or rectum due to genetic mutations, typically progressing from benign polyps (adenomas) through the adenoma-carcinoma sequence involving Wnt signaling pathway alternations.
Causes and Risk Factors
Primary causes include genetic mutations (inherited like Lynch syndrome or acquired), lifestyle factors such as high red meat intake, low fiber diet, smoking, obesity, alcohol, and sedentary behavior; risk rises with age over 50, family history, inflammatory bowel disease, and type 2 diabetes.
The main risk factors for colorectal cancer include both modifiable lifestyle elements and non-modifiable factors like age and genetics.
Modifiable Lifestyle Factors
These are largely preventable through diet and behavior changes. Key ones are diets high in processed/red meats and low in fruits/vegetables/fiber, physical inactivity, obesity, heavy alcohol use, and smoking/tobacco exposure.
Genetic Factors
Inherited syndromes like Lynch syndrome (HNPCC) or familial adenomatous polyposis (FAP) greatly elevate risk, as does family history. A personal history of colorectal polyps, previous cancer, and inflammatory bowel disease also increases odds.
Main Types
Adenocarcinoma (most common, ~95%, from glandular cells).
Others: carcinoid tumors, gastrointestinal stromal tumors (GIST), lymphomas, and sarcomas.
Symptoms
Early stages are often asymptomatic; later signs include blood in stool, persistent diarrhea, constipation, abdominal pain, cramps, ongoing belly pain, gas that doesn’t resolve, unexplained weight loss, fatigue, anemia (iron deficiency), and bowel habit changes.
Diagnosis and Methods
Diagnosis starts with symptom evaluation and is confirmed via colonoscopy (the gold standard for visualization and biopsy).
Other methods: fecal occult blood test (FOBT), FIT, sigmoidoscopy, CT colonography, blood tests (CEA marker), biopsy for staging (TNM system), and imaging (CT/MRI/PET scans).
Prevention Measures
Screening from age 45 (earlier if high-risk) via colonoscopy every ten years or stool tests annually removes precancerous polyps.
Lifestyle: high-fiber diet (fruits/veggies), limit processed meats, alcohol, exercise, maintain healthy weight, quit smoking.
Control Measures
Population screening programs reduce incidence/mortality by 20% to 30%; vector control is irrelevant here, but surveillance via registries tracks trends.
Early detection via organized programs (e.g., WHO-recommended) and polyp removal is key.
Treatment
Depends on stage: surgery (polypectomy, colectomy), chemotherapy (e.g., FOLFOX), radiation (rectal cancer), targeted therapy (anti-EGFR like cetuximab), immunotherapy (pembrolizumab for MSI-high).
Early-stage cure rates > 90%, advanced ~ 14% 5-year survival.
Public Awareness
Campaigns emphasize “no symptoms doesn’t mean no cancer”; promote screening myths busting (e.g., “it’s only for old people”). Use social media and survivor stories; WHO notes rising young adult cases needing awareness.
Community Engagement
Local events, support groups, and faith-based outreach for screening uptake; partner with NGOs for mobile clinics in underserved areas like rural India.
IEC Materials
Information, education, and communication tools: posters on symptoms, screening, pamphlets in local languages, videos on colonoscopy prep, and apps for risk calculators.
Role of Public Health Department
Departments lead screening programs, fund surveillance, train health providers, enforce tobacco and alcohol policies, run awareness drives, integrate into NCD programs (e.g., India’s NPCDCS), and monitor outcomes via cancer registries.
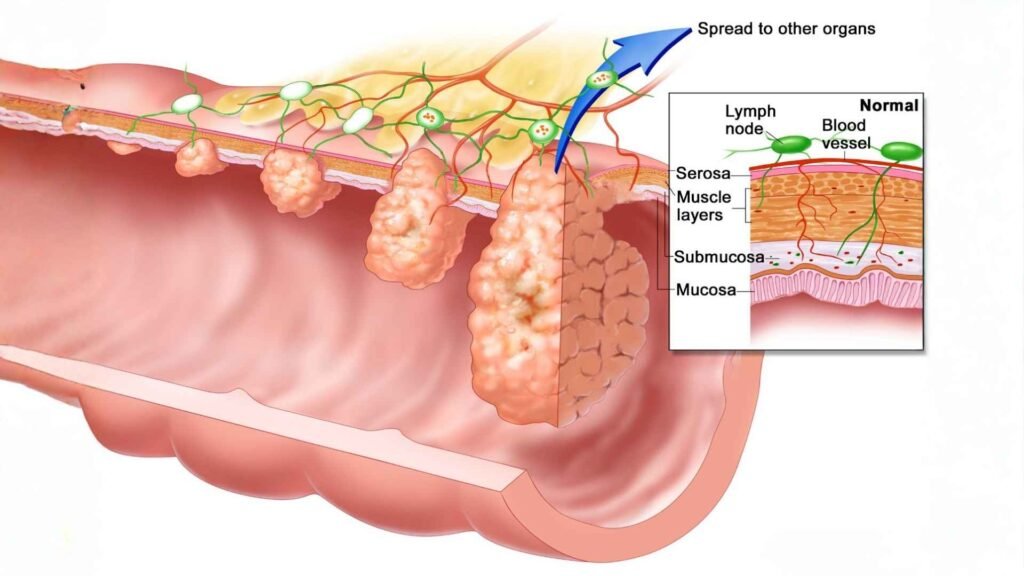
Stages of Colon Cancer
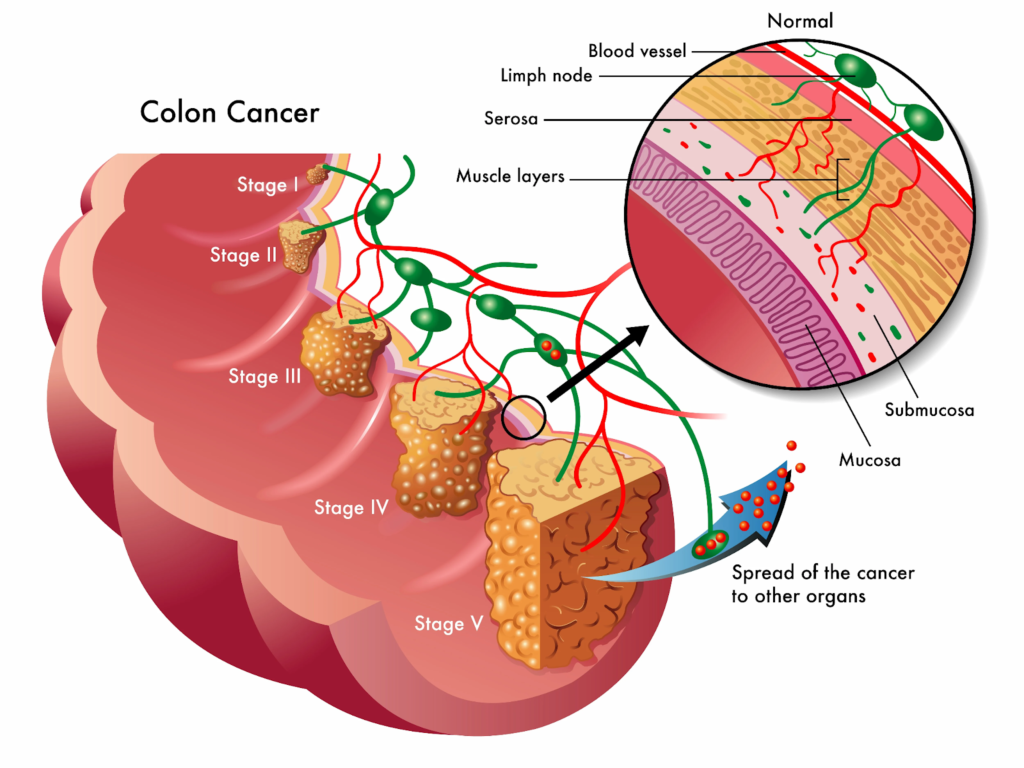
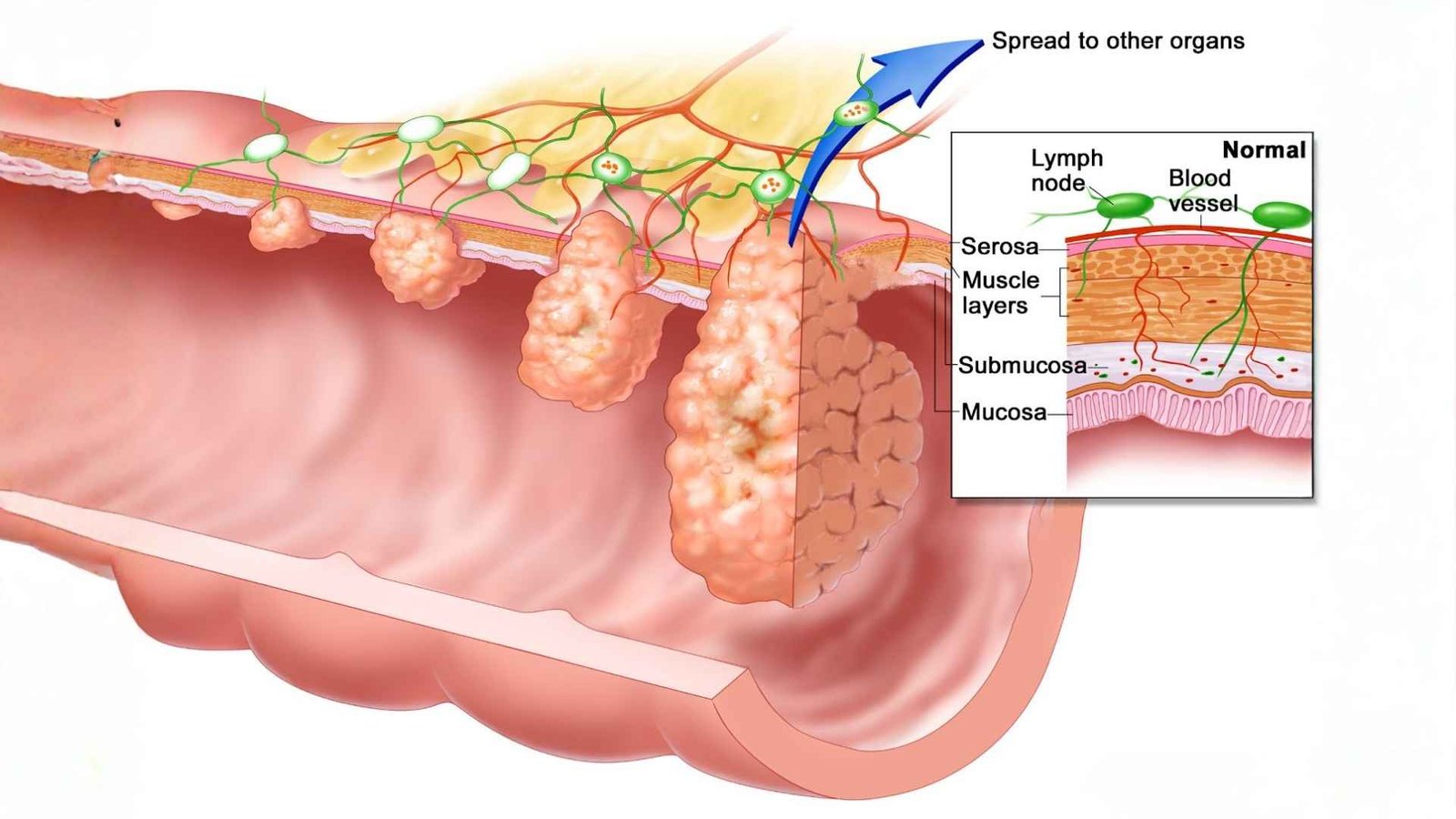
Colon cancer, also known as colorectal cancer, is staged from 1 to 5 based on how far it has spread through the colon wall, to lymph nodes, or to distant sites.
Staging uses the TNM system (Tumor, Node, Metastasis) to guide treatment and prognosis.
Stage 1
Cancer is confined to the innermost lining (mucosa) of the colon and hasn’t invaded deeper layers. It’s often called carcinoma in situ and is highly treatable with surgery alone.
Stage 2
The tumor has grown into the submucosa or muscularis propria but hasn’t reached lymph nodes or distant sites. Surgery is typically curative with excellent outcomes.
Stage 3
Cancer has penetrated the outer layers of the colon wall (substages 2A, 2B, 2C) but not lymph nodes. It may reach nearby tissues or the peritoneum: adjuvant chemotherapy is sometimes added post-surgery.
Stage 4
The tumor has spread to nearby lymph nodes (substages 3A, 3B, 3C) but not distant organs. Treatment combines surgery, chemotherapy, and often targeted therapies based on node involvement.
Stage 5
Cancer has metastasized to distant sites like the liver, lungs, or peritoneum (substages 4A, 4B, 4C). Management is systemic with chemotherapy, plus surgery if feasible.
Stage Summary Table
| Stage | Key Spread | Common Treatment |
|---|---|---|
| 1 | Mucosa only | Local excision |
| 2 | Submucosa/muscle | Surgery |
| 3 | Outer wall | Surgery + Chemo |
| 4 | Lymph nodes | Surgery + Chemo |
| 5 | Distant Organs | Systemic therapy |