Bladder cancer is a disease where malignant cells form in the tissues of the bladder, the organ that stores urine. It most commonly starts in the inner lining cells called urothelial or transitional cells.
Definition
Bladder cancer involves abnormal growth of cells in the bladder, forming tumors that can invade deeper layers and spread to other organs if untreated. Most cases (about 90%) are urothelial carcinomas originating from the bladder’s lining.
Causes
It arises from DNA changes in bladder cells, often acquired during life rather than inherited. Key triggers include tobacco smoke chemicals filtered into urine, workplace exposures to dyes, paints, metals, or petroleum, and certain gene mutations like HRAS or RB1.
Main Types
Urothelial (transitional cell) carcinoma: 90% of cases start in lining cells
Squamous cell carcinoma: 4% from chronic irritation
Adenocarcinoma: 2% glandular cells
Small cell carcinoma and sarcoma: rare, aggressive types.
Symptoms
Common signs include blood in urine (hematuria), frequent or urgent urination, pain or burning during urination, urinary tract infections, back or lower abdominal pain, unexplained weight loss, fatigue, and bone pain.
Diagnosis
Diagnosis begins with evaluating symptoms like hematuria, followed by cystoscopy (camera inspection of bladder) and biopsy of suspicious tissues. Urine cytology checks for cancer cells, while imaging like CT urography assesses spread.
Diagnosis Methods
Primary methods: cystoscopy with biopsy (gold standard), urine cytology, fluorescence in situ hybridization, tumor markers (BTA, NMP22), and imaging (ultrasound, CT/MR). Combined urine markers and cytology boost sensitivity to 95%.
Prevention Measures
Quit smoking (major risk reducer), stay hydrated to flush toxins, eat fruits/vegetables while limiting red meat/fats, avoid chemical exposures at work, and get regular check-ups if high-risk (family history, prior infections).
Control Measures
Early screening in high-risk groups via NPCDCS in India (for common cancers, adaptable to bladder), tobacco control, occupational safety, and post-treatment surveillance reduce recurrence. Public campaigns promote early detection to lower mortality.
Treatment
Depends on the stage: transurethral resection (TURBT) for early tumors, intravesical BCG immunotherapy, cystectomy (bladder removal), chemotherapy (cisplatin-based), radiation, or immunotherapy like pembrolizumab with enfortumab vedotin.
Public Awareness and Community Engagement
Awareness campaigns use symposiums, booths, social media, walks (e.g., May Bladder Cancer Awareness Month), and surveys to educate on risks/smoking. Community events in public areas like clinics boost knowledge from 60% to 95% on diagnosis/treatment.
IEC Materials
Posters, social media graphics, brochures, and online videos highlight symptoms, risks (smoking, chemicals), screening, and early detection. Tailored for rural/suburban groups, they empower self-checks and support groups.
Role of Public Health Department
In India, departments under NPCDCS strengthen screening/treatment facilities, fund tertiary cancer centers, run NCD programs, collaborate with networks like NCG for 60% cancer burden coverage, and promote Ayushman Bharat for affordable care.
Prognosis and Survival Rates for Bladder Cancer Stages
Bladder cancer survival rates vary significantly by stage at diagnosis, with early detection offering the best prognosis. These are typically reported as 5-year relative survival rates from sources like the National Cancer Institute (NCI) and American Cancer Society (ACS), based on recent data from 2015 to 2021.
Survival By Stage
Survival drops as cancer advances beyond the bladder. Here’s a breakdown using SEER staging (localized: confined to bladder): regional: nearby spread; distant metastatic)
| Stage | 5-year Relative Survival Rate | Description |
| In Situ (non-invasive) | 97% to 98% | Abnormal cells in lining only, highly treatable |
| Localized (Stage 0-I) | 70% to 75% | Tumor in bladder wall, no spread |
| Regional (stage II-III) | 39% to 41% | Spread to nearby tissues/lymph nodes |
| Distant (Stage IV) | 8% to 9% | Metastatic to distant organs |
| All stages combined | 78% to 79% | Overall average across diagnosis. |
Prognosis Factors
Prognosis improves with early intervention like TURBT or BCG therapy for non-muscle-invasive cases (over 90% initial 5-year survival in some stages 0 to I reports). Key influencers include age, overall health, tumor grade, smoking cessation, and new treatments like immunotherapy, which boost outcomes beyond historical rates. Individuals’ results vary; consult oncologists for personalized estimates. Older age worsens prognosis due to declining immunity and comorbidities, e.g., heart disease and diabetes. and higher carcinogen exposure over time. Race and sex show minor impacts in some studies, with non-Hispanic whites often having a higher incidence but variable survival.
Palliative Care for Bladder Cancer
Palliative care for bladder cancer focuses on relieving symptoms and improving quality of life, often alongside active treatments. It addresses pain, fatigue, nausea, urinary issues, and emotional distress from advanced or metastatic disease. Teams manage common issues like pain, shortness of breath, constipation, loss of appetite, and sleep problems with medications, therapies, or procedures such as urinary diversion. Psychological support tackles anxiety and depression early, even at diagnosis, not just at end stage. Nutritionists and social workers help with practical needs like diet and home care. Palliative care starts anytime, from diagnosis through metastasis, complementing chemo, radiation, or immunotherapy.
Care Team Role
Multidisciplinary groups include doctors, nurses, and specialists who align treatments with patient values. Early involvement aids decisions on surgery or therapy burdens versus disease effects. Patients often want more discussions on this during treatment planning.
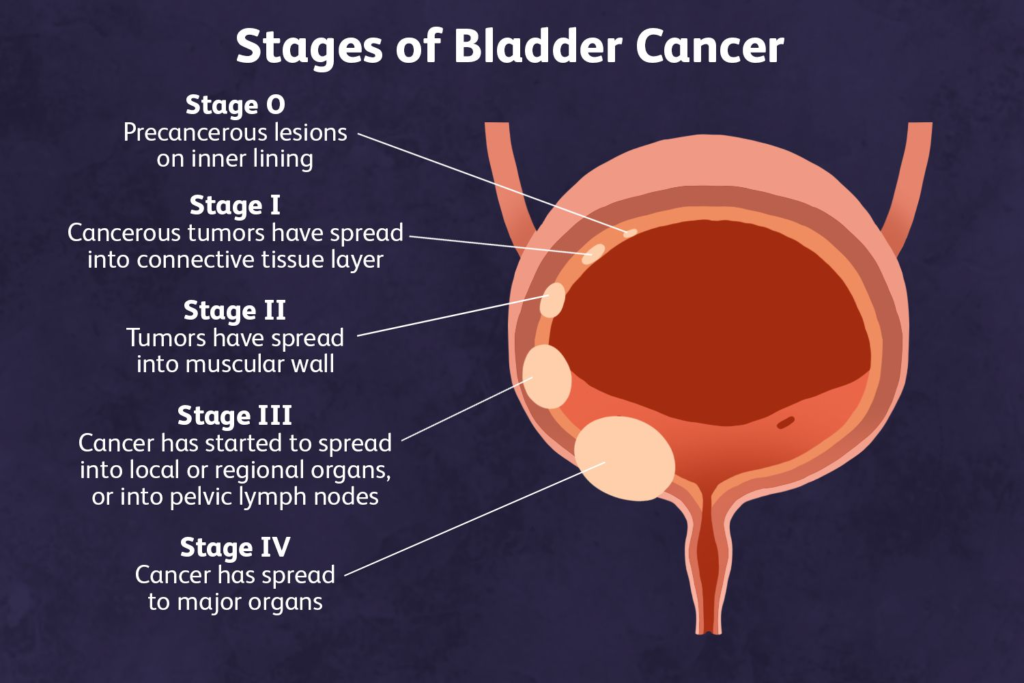
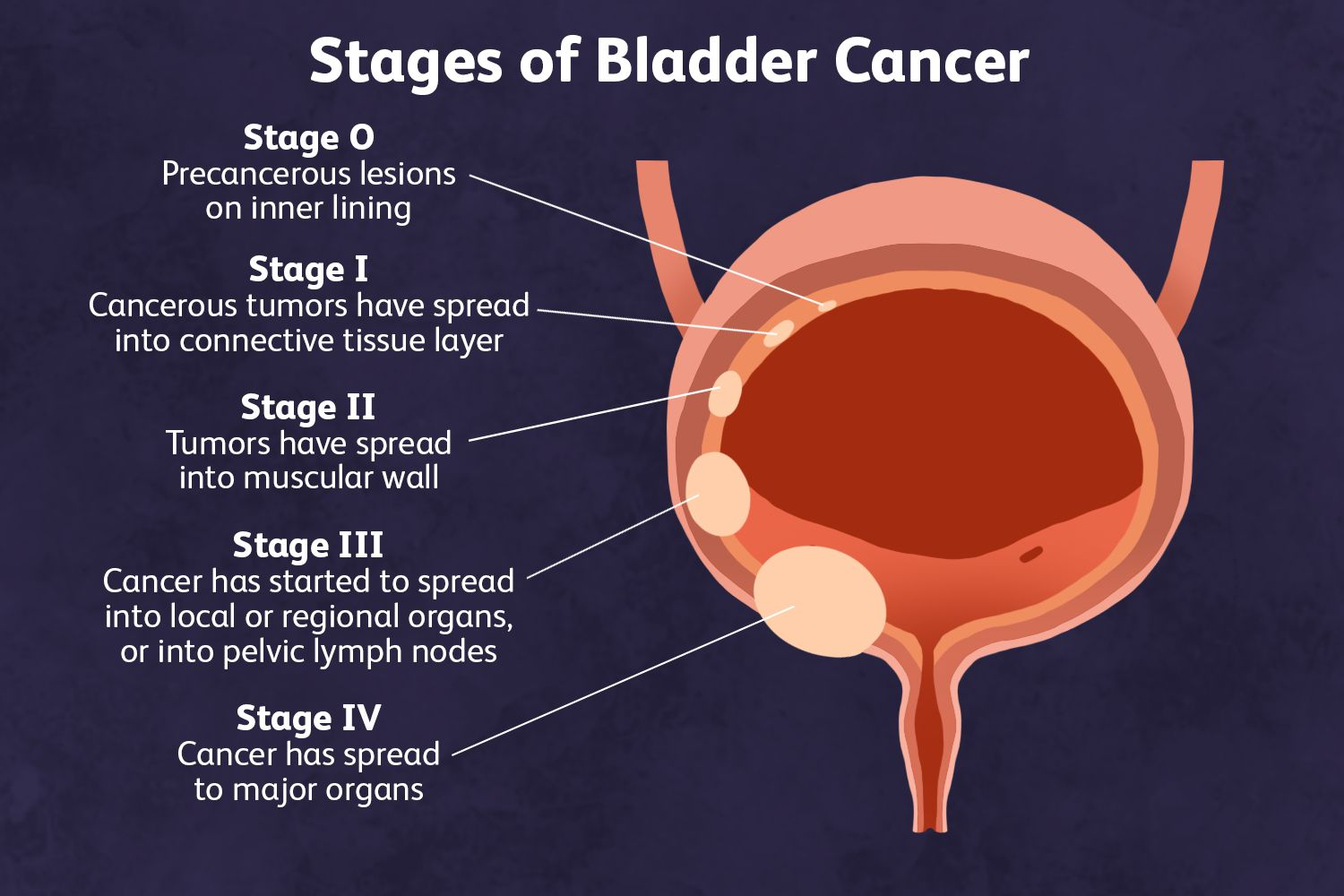
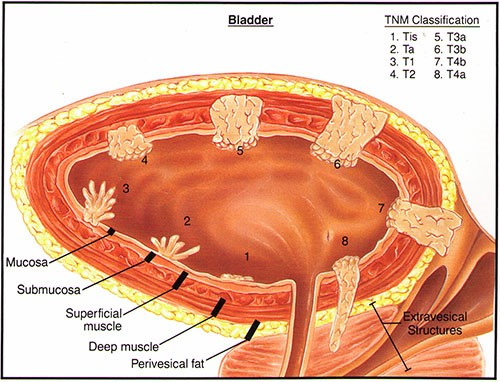
Stages of Bladder Cancer
Bladder cancer is staged using systems like TNM (tumor, node,Metastasis ) or numbered stages from 0 to 4 to describe its extent and spread. Staging helps to determine treatment by assessing tumor depth, lymph node involvement, and distant spread. The TNM system details this:
1) T describes tumor invasion into bladder layers
2) N covers nearby lymph nodes (N0 none, N1-N3 increasing spread).
3) M indicates metastasis (M0 none, M1 present).
Stage 0: Cancer is confined to the bladder’s inner lining surface (Ta or carcinoma in situ / Tis). It hasn’t invaded deeper layers.
Stage 1: The tumor has grown into the connective tissue beneath the lining (T1) but not the muscle .No lymph node or distant spread.
Stage 2: Cancer invades the bladder muscle wall (T2, split into superficial T2a or deeper T2b). Still no spread beyond the bladder
Stage 3: The tumor extends through muscle into surrounding fat (T3, microscopic T3a, or visible T3b) or nearby organs/lymph nodes, but not distant sites.
Stage 4: Advanced cancer has spread to pelvic/abdominal walls, distant lymph nodes, or organs like lungs, liver, or bones (T4 or M1).