The World Health Organization has included the use of the tourniquet test for the diagnosis of dengue infection. The accuracy of the tourniquet test for dengue fever varies, with some studies showing a sensitivity of around 90% and a specificity of about 72%, while others report a lower sensitivity of around 60% and a higher specificity of around 72%. It has limitations, such as low sensitivity in certain populations. Therefore, it’s best used as a simple, inexpensive triage tool in resource-limited settings.
- Sensitivity: Some studies shows high sensitivity around 90%
- Specificity: Some studies report a specificity ranging from 70% to 92%.
- Success rate of test: The survival rate was also higher if the tourniquet was placed prior to the onset of shock; 92% of those patients survived the injuries in comparison to only 18% of those with tourniquets placed after the onset of shock.
The normal value of the tourniquet test
The test is positive if there are more than 10 to 20 petechiae per square inch. Normally less than 15 petechiae are seen in a 5 cm diameter circle of the area under pressure.
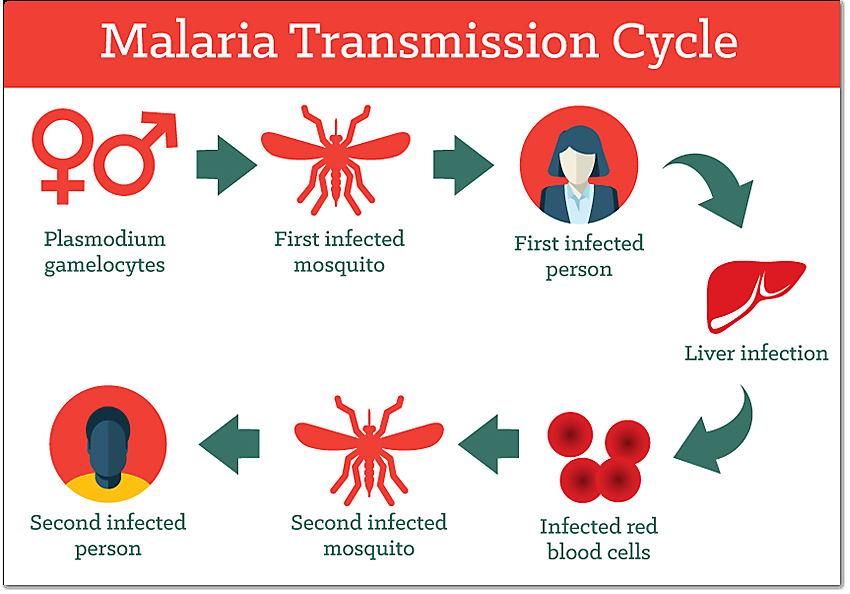
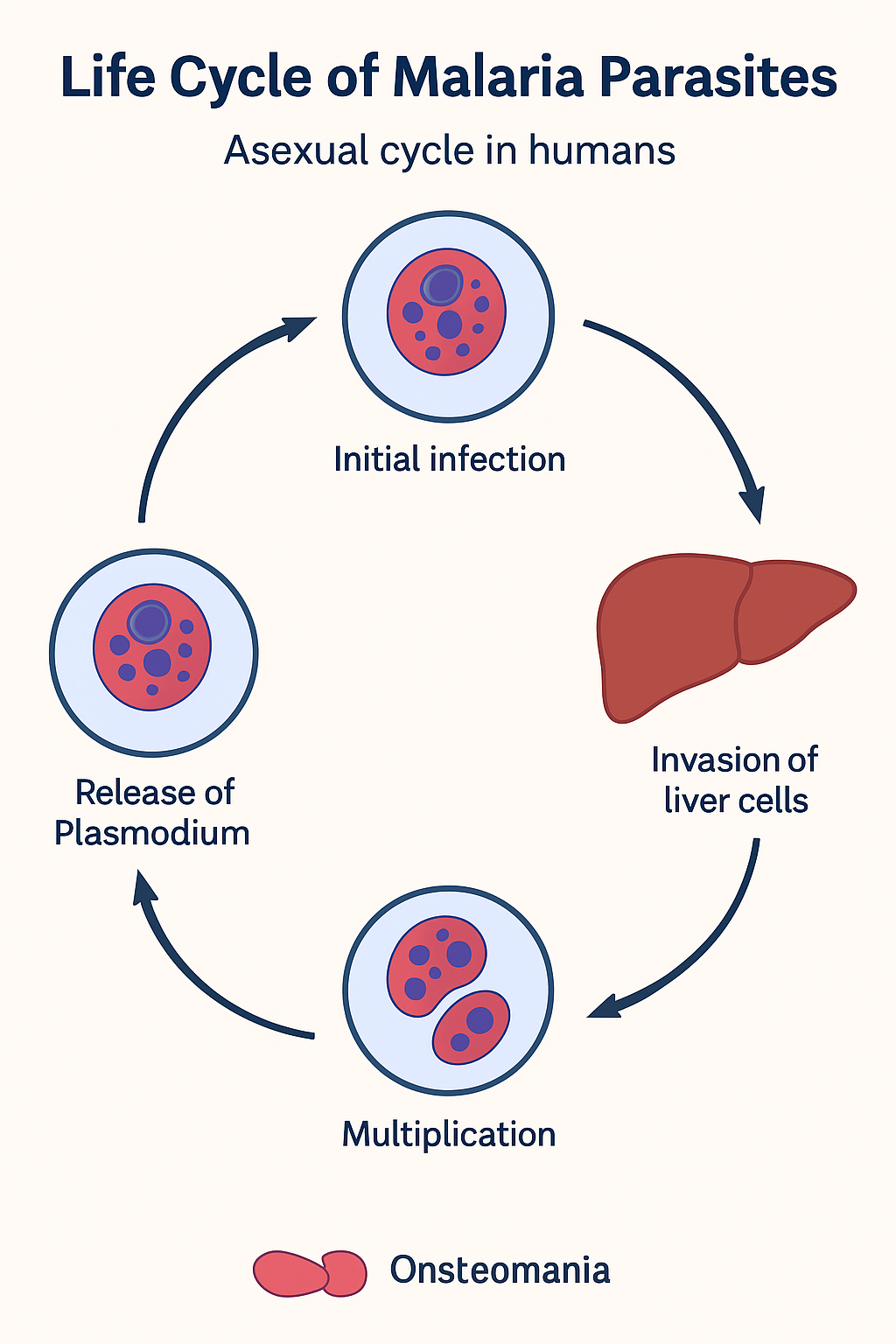
Dengue fever is dangerous during the critical phase, which typically occurs 24 to 48 hours after the fever breaks, around 3 to 7 days of illness. During this time severe warning signs, such as intense abdominal pain, persistent vomiting, bleeding from gums or nose, or difficulty breathing, can indicate that the illness is progressing to severe dengue. Such as dengue shock syndrome.
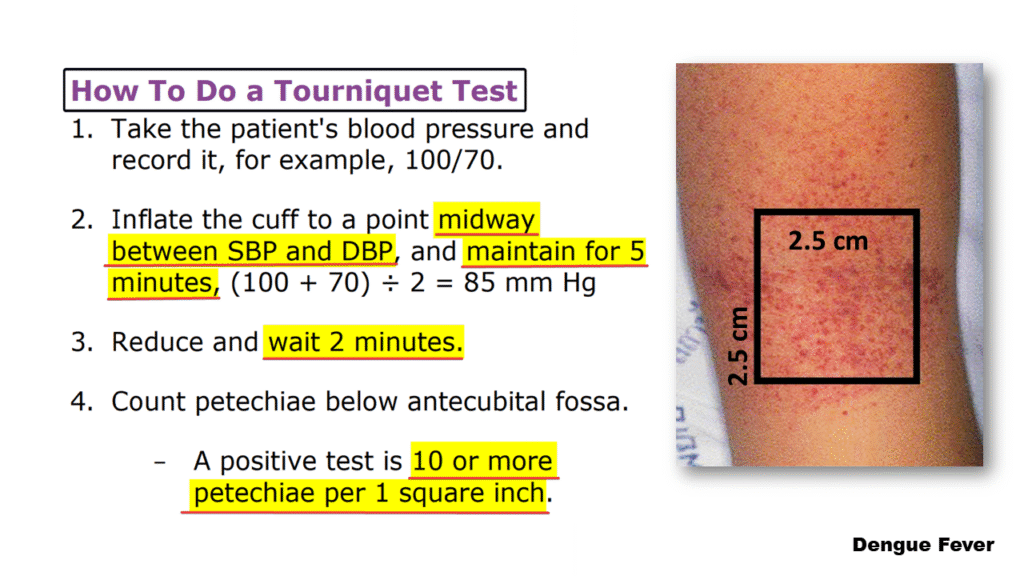
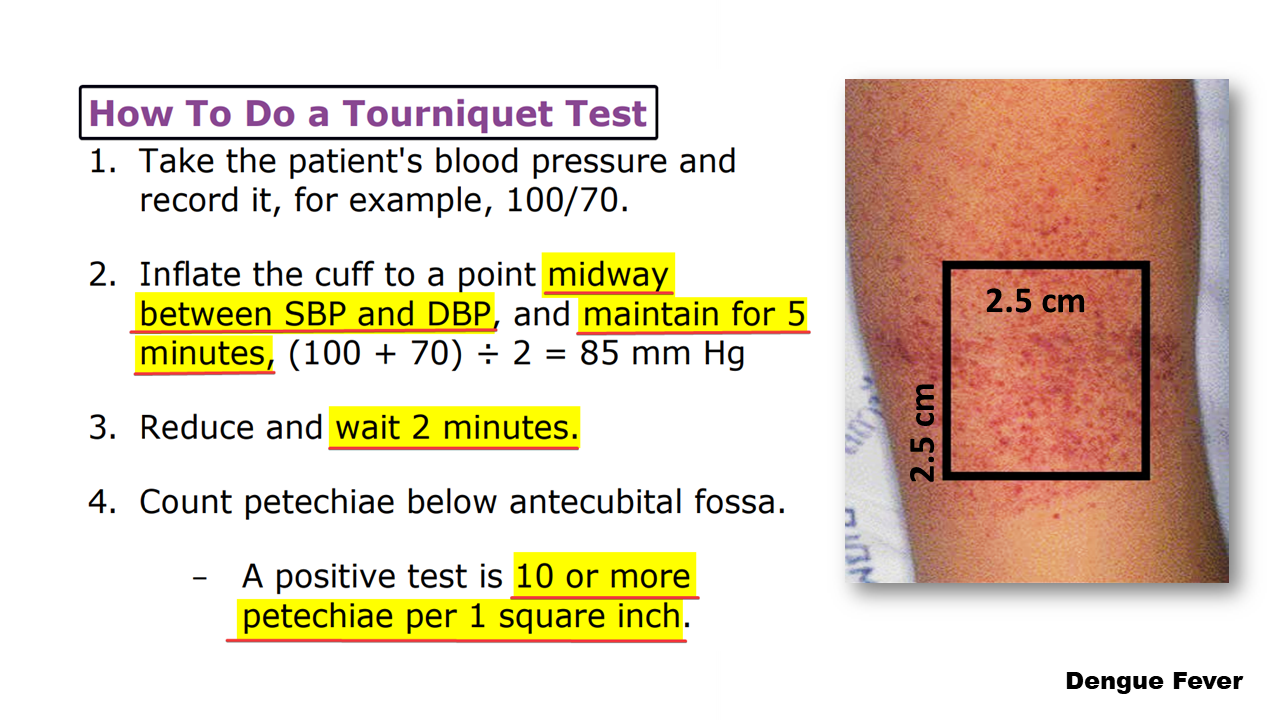
The following important steps for performing a tourniquet test are
1) Record blood pressure
Doctors first measure and record the patient’s blood pressure (BP) to determine the systolic and diastolic values of the readings.
2) Inflate the blood pressure cuff
Inflate a blood pressure cuff on the upper arm to a pressure midway between the systolic and diastolic blood pressures. e.g., if BP is 120/80, inflate to 100 mmHg.
3) Maintain pressure
The blood pressure is maintained for five minutes exactly, without causing undue discomfort.
4) Deflate the cuff
After the five minutes, the cuff is deflated, and the doctor waits for two minutes.
5) Count petechiae
The doctor then inspects the patient’s forearm below the cuff and counts the number of petechiae in a standardized area such as a 2.5 cm square (i.e., typically 2.5 cm by 2.5 cm).
6) Interpret the result
Count the number of petechiae (tiny purplish areas or red spots caused by capillary bleeding) appearing in this marked area. A positive result is considered to be 10 or more petechiae in the 2.5 cm² area, indicating a positive tourniquet test, reflecting capillary fragility and thrombocytopenia; it is commonly seen in dengue fever. In dengue hemorrhagic fever (DHF), 20 or more petechiae may be seen.
Negative
Fewer than 10 petechiae.
Thus, this test assists in diagnosing dengue, especially hemorrhagic manifestations, and helps to guide early clinical management of severe cases. It is recommended to repeat the test if initially negative but clinically suspicious.
Remains high The tourniquet test is usually positive in DHF but can be negative or mildly positive during profound shock in dengue syndrome (SSD).
Purpose of the Tourniquet Test
The tourniquet test is a measure of capillary fragility and helps in diagnosing dengue hemorrhagic fever. The appearance of the numerous petechiae, which are tiny hemorrhages under the skin, suggests that the patient’s capillaries are weakened and more prone to bleeding.
Formula for Tourniquet Test
(Systolic blood pressure + diastolic blood pressure) for a minute / 2 = we get the answer.
Here,
1) Reduce and wait two minutes.
2) A positive test is 10 or more petechiae per 1 square inch.