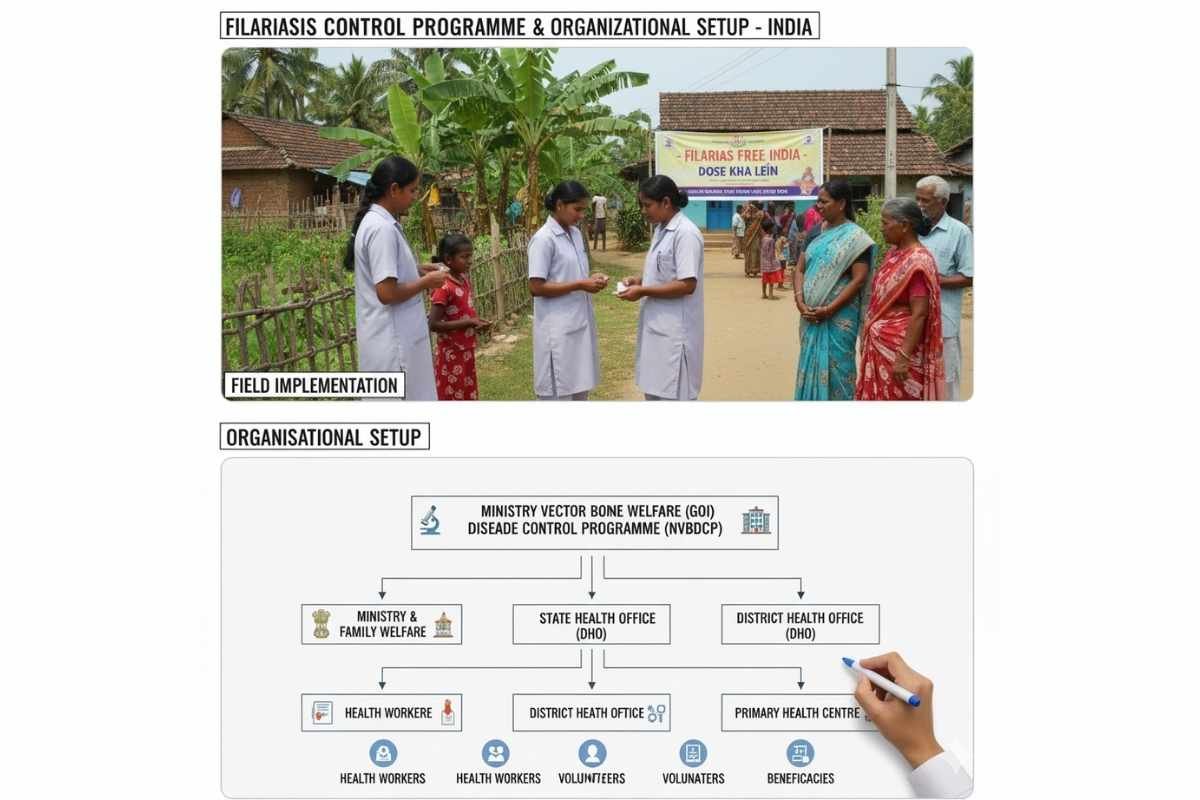
The National Filaria Control Programme (NFCP) was started in 1955 under the National Institute of Communicable Diseases (NICD), Delhi, with the following objectives:
- Delineation surveys in known endemic areas.
- Large-scale control measures in selected areas.
- Training of personnel required to man the program.
The NFCP was transferred from NICD to the National Malaria Eradication Programme (NMEP) in 1978. The NFCP was evaluated four times by appointed assessment committees in 1961, 1971, 1982, and 1995.
Organizational Setup
Central Level
The central-level organization for training and research on filariasis consists of a Joint Director, other officers, and staff at the National Institute of Communicable Diseases (NICD), Delhi. There are three Regional Filaria Training & Research Centres (RFTRC) located at Kozhikode in Kerala, Rajahmundry in Andhra Pradesh, and Varanasi in Uttar Pradesh. Each RFTRC is headed by an Assistant Director or Joint Director with supporting officers and other staff. The NFCP is under the Director of the National Centre for Vector Borne Diseases Control (NCVBDC) (formerly known as NVBDCP), Delhi.
The important functions of the Central organization are
- To plan, coordinate, and evaluate according to the pattern, and to offer financial and technical guidance to States/Union Territories (UTs) for the implementation of the program.
- To train officers and staff.
- To undertake research studies on epidemiology, newer methods of filaria control, and related aspects.
A Central Filaria Survey Team was established in 1970 and located at NICD, Delhi, which monitors filaria transmission in selected areas in non-endemic states. Research on Brugia malayi was undertaken by the NICD through its branch, the B. malayi Research Unit, located at Shertallai in Kerala.
State Level
The NFCP in each of the 18 endemic States/UTs is led by a Joint Director (Malaria/Filaria), with supporting staff including a State Entomologist, a State Assistant Director of Health Services (Filaria), and other officers and staff. States have been requested to identify an Assistant Director of Health Services (Malaria) at the division level and a District Malaria Officer or Filaria Officer at the district level for all vector-borne disease control. This is intended for better coordination of vector-borne disease control at the division and district levels, respectively.
The role of Filaria Control Units, Survey Units, and Filaria Night Clinics, along with their staffing pattern as per Government of India (GOI) norms:
a) Filaria Control Unit (FCU)
The FCU primarily involves implementing control measures to eliminate lymphatic filariasis in endemic areas. These units are responsible for organizing primary anti-larval measures, such as weekly larval source reduction (e.g., filling ditches, de-weeding, de-silting). They also implement biological control using larvivorous fish and undertake vector control activities to reduce the density of mosquitoes that transmit the disease. These units help reduce hydrocele cases primarily through the Morbidity Management and Disability Prevention (MMDP) programme , which includes surgical operation and treatment (hydrocelectomy). Other elephantiasis patients receive training on limb care techniques, limb elevation, exercise, proper hygiene, and skin care to prevent secondary infection from health workers. In these units, insect collectors collect mosquitoes, usually female mosquitoes. These are sorted and morphologically identified to the species level. Then, under a dissecting microscope, mosquitoes are dissected and different parts, such as the head, thorax, and abdomen, are removed for examination. This is done to detect infection and infectivity by checking for the presence of microfilariae (mf) or larval stages (L-1, L-2, L-3). All vector parameters are then calculated for accurate monitoring of filariasis transmission. The FCUs also conduct routine night blood surveys for microfilaria carrier detection within target populations for the evaluation of anti-larval measures. They provide treatment to mf carrier patients with drugs such as DEC, Ivermectin, and Albendazole, according to age-wise and height-wise schedules. The Control Unit team conducts night blood surveys covering 10% of the population, specifically during night hours, especially 8:30 PM to midnight (12:00 AM). These sub-units have two teams, and each team should undertake the survey for three or four nights per month. * For Random (Spot-check) blood sample collection: 75 blood smears (BS)×2 teams×1 night=150 BS. * For Fixed (Sentinal) blood sample collection: 75 BS×2 teams×3 nights=450 BS. The total target of blood smear collection against 10% of the population is 600 per sub-unit. If there are two Filaria Inspectors or Health Assistants per sub-unit, two survey teams can be formed. If each team works for 24 nights in a year for the survey, the number of team-nights is 48. Therefore, 48 beats or maps are to be selected. Thus, one round is to be completed within a year for 50,000 population, as per the sub-units. These units also contribute to education and community engagement efforts to support personal protective and preventive practices against filaria transmission. They also conduct Mass Drug Administration (MDA) or Ivermectin-Diethylcarbamazine-Albendazole (IDA) programmes. Thus, the FCU implements anti-larval measures, vector control, biological control, morbidity management, hydrocele patient operation, and subsequent night blood surveys for assessment.
b) National Filaria Survey Unit (NFSU)
The Filaria Survey Units (FSUs) systematically conduct Night Blood Surveys (NBS) to determine microfilaria rates and identify filariasis endemic areas. They do this by collecting night blood samples covering 100% of the population and detecting microfilaria carriers. They gather epidemiological data necessary for assessing disease burden and transmission patterns. Infected patients (mf carriers) are treated through Primary Health Centre (PHC) level staff, and follow-up is carried out at their level. Based on the findings of the Filaria Survey Units, Filaria Control Units, sub-units, and Filaria Night Clinics are established for further necessary activities. Maharashtra runs a total of six dedicated Filaria Survey Units throughout the endemic region. These are supplemented by 16 FCUs, 13 Night Clinics, and one training centre, according to the programme documentation. The Filaria Survey Team has completed the initial survey, and a re-survey is currently in progress. Among two teams, each team can collect smears from about 75 persons, and two teams are expected to cover about 3,000 blood smears in a month. The team would plan two continuous tours of 12 days each, which should provide 20 survey nights in a month. This translates to 5 days×2 teams=10 working nights. The Filaria Officer in the NFSU should accompany the team alternately to improve the progress and quality of work. The Filaria Officer is to cross-check 5% to 10% of blood smears every day and confirm the density of mf and species. A Filaria Survey Unit should survey 200 nights in a year , meaning not less than 200 nights are spent on the surveys in a year. At least 14 houses should be chosen for each village selected, and at least 75 blood smears should be collected per survey night by each team.
c) Filaria Night Clinic (FNC)
Night clinics are established to enhance access to early diagnosis, complete treatment, regular follow-up, and treatment of lymphatic filariasis cases (i.e., disease cases like elephantiasis). They also provide morbidity management, including the care of lymphedema and hydrocele cases in endemic rural or urban areas. The total population under each Filaria Clinic would be about 50,000, and the screening of the total population will take about two and a half years. 1,500 blood smears should be taken each month. House-to-house visits would be made five nights a week. A clinic would be established on the sixth night of the week. All members of the household would be examined for evidence of acute or chronic manifestation of filariasis. A team can examine and collect blood smears from about 75 persons in a night , and the survey could be done for 20 nights in a month. Thus, about 1,500 persons or blood smears are expected to be examined in a month. At least 90% of the enumerated population should have a blood film taken (i.e., collecting night blood samples covering 100% of the population). A drug distributor can attend to or treat 60–70 persons per day.