Breast cancer involves uncontrolled growth of abnormal cells in breast tissue, often forming tumors that can spread if untreated. These brief notes cover its key aspects for quick reference. It primarily affects women but occurs in men rarely, with early detection improving outcomes significantly.
Definition
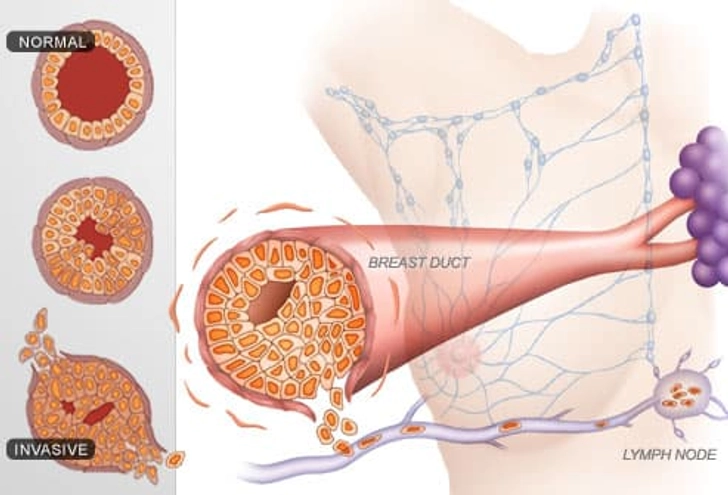
Breast cancer is a malignancy originating in breast cells, typically in milk ducts (ductal carcinoma) or lobules (lobular carcinoma).
Types
Common types include ductal carcinoma in situ (DCIS, non-invasive), invasive ductal carcinoma (most frequent, spreads beyond ducts), invasive lobular carcinoma, and rare forms like inflammatory or triple-negative breast cancer.
Causes
Primary causes link to genetic mutations, e.g., BRCA 1 and BRCA 2 genes, but risk factors include age over 50, family history, dense breasts, hormone therapy, obesity, alcohol use, and lack of physical activity; exact triggers often remain unknown.
Stages
Staging ranges from 0 (in situ, confined to ducts/lobules) to IV (metastatic, spread to distant organs).
Stages I to II are early/localized.
Stages III locally advanced
Stages IV advanced
Symptoms
Key signs are a painless lump, breast thickening, nipple changes (inversion, discharge), skin dimpling/redness, or swollen lymph nodes; early stages may be asymptomatic.
Common Symptoms
New lump or thickening in the breast, chest, or underarms (armpit), often painless.
Changes in the breast size, shape, or symmetry, such as swelling or heaviness.
Skin changes like dimpling (“orange peel” texture), redness, flaking, irritation, or puckering.
Nipple-Related Signs
- Nipple inversion (pulling inward), pain or retraction
- Discharge from the nipple (clear, bloody, or not breast milk).
- Persistent breast or nipple pain/tenderness.
- Swollen lymph nodes under the arm or near the collarbone.
Diagnosis

Breast cancer screening and diagnosis involve imaging for early detection and confirmatory tests when abnormalities are found. These methods help identify the disease before symptoms appear or confirm it after suspicion.
Signs Of Inflammatory Breast Cancer
Screening Methods
Screening aims at early detection in asymptomatic women. Mammography is the primary tool, recommended annually or biennially starting at age 40 to 50 depending on risk; digital breast tomosynthesis (3D mammography) improves accuracy over 2D.
Clinical breast exams by providers and self-exams are supplementary but are less sensitive alone; MRI is advised for high-risk women, e.g., BRCA carriers. MRI provides detailed imaging for dense breasts or staging. Biopsy is definitive, examining cells for cancer type and markers like hormone receptors or HER2. Diagnosis follows screening, like lumps. Ultrasound distinguishes cysts from solids.
Treatment
Options depend on stages/type and include surgery (e.g., lumpectomy, mastectomy), radiation, chemotherapy, hormone therapy (e.g., tamoxifen for ER-positive), targeted therapy (e.g., HER2 inhibitors), and immunotherapy; early detection improves outcomes.
Risk Factors
Breast cancer risk factors include both unchangeable and modifiable elements, while prevention focuses on lifestyle adjustments and early detection.
1) Non-modifiable
Age (risk rises after 50 yrs), female sex, family history, especially first-degree relatives, genetic mutations like BRCA1/BRCA2, dense breast tissue, early menstruation (before age 12), late menopause (after 55), and prior radiation exposure.
2) Modifiable
Obesity (post menopause), alcohol consumption, physical inactivity, hormone replacement therapy (estrogen-progesterone combos), never breastfeeding or late first pregnancy (after 30 years), smoking, and high red/processed meat intake.
Prevention
Maintain a healthy weight through a balanced diet and exercise; aim for 150+ minutes of moderate activity weekly.
Limit alcohol to one drink per day or less; avoid smoking.
Breastfeeding, if possible, even for months, reduces risk; eat more fruits, vegetables, and whole grains while cutting saturated fats.
Undergo regular screenings like mammograms starting at age 40-50 (earlier if high-risk); ); consider genetic counseling for BRCA testing if a family history exists.
Limitations and Sensitivity of Mammography
Mammography is the gold standard, the primary method for breast cancer screening, and effectively reduces mortality by detecting cancers early, but it is not perfect, though it has limitations like false positives and reduced sensitivity in dense breasts.
Sensitivity
Typically 70% to 90% for detecting breast cancer, meaning it identifies most invasive cancers but misses 10% to 30% (i.e., false negatives). Sensitivity drops to ~ 60% to 80% in women with dense breasts, as tumors can blend with glandular tissue. Example: In a study of 100 women with cancer, it might detect 85 but miss 15.
Limitations
Dense breasts: Reduces visibility; up to 40% to 50% of premenopausal women have dense tissue.
False Positive: 7% to 12% per screening, leading to anxiety; biopsies are unnecessary in ~ 1%.
Internal Cancer: 20% to 30% of cancers appear between screenings.
Detection Gaps: Misses ~ 15% to 20% of ductal carcinoma in situ (DCIS is ); less effective for lobular cancers).
Radiation exposure: Low dose of ~ 0.4 mSv per exam, like 7 weeks of background radiation, but cumulative risk.
Not Ideal For All: Younger women (< 40 yrs.) and high-risk groups may need MIR/ultrasound adjuncts.
For better accuracy, combine with clinical exams, ultrasound, or 3D tomosynthesis. Guidelines recommend biennial screening for average-risk women 50% to 80%.
Self Breast Examination Step by Step
Breast self-exams help you spot changes early, though they are not a substitute for professional screening like mammograms. Perform one monthly, ideally 7 to 10 days after your period starts.
Visual Inspection
Stand in front of a mirror with arms at sides, then overhead and hands on hips, pressing firmly. Look for changes in size, shape, symmetry, skin dimpling, redness, nipple inversion, or swelling in breasts/underarms.
Public Awareness
Awareness campaigns highlight early symptoms, promoting breast self-exams, screening, and then early medical seeking.
Community Engagement
Healthcare providers and NGOs are using flipcharts, models, and PowerPoint on symptoms, risk, and screening for high-risk groups and patient stories to foster support.
Role of Public Health Department
Public health departments play a pivotal role in breast cancer prevention, surveillance, early detection, and control through policy implementation, community programs, and infrastructure support.
In India, including Maharashtra, they integrate these efforts into national NPCDCS departments. They screen via trained ASHA and ANM workers, provide referrals and treatment at district hospitals, and integrate awareness into routine visit activity.